A Decade of Value-based Care - How was it? Are Healthcare Organizations Caring as One?

It has been almost a decade since the government passed the Affordable Care Act (ACA). The healthcare industry has learned a lot in this period of payment reforms and administrative changes. Yet, have we implemented the operational shifts needed for true value-based care? Whether or not there is a longing for the simpler times of fee-for-service medicine is debatable, one thing is for sure — value-based care is here to stay — and it’s likely to become more entrenched in the decade to come.
Healthcare organizations and providers face increasing complexities in the process of delivering good medical care. Their daily patient care activities continue to be hamstrung by overwhelming and redundant administrative work.
There is an evolution underway to reinvent the way healthcare teams use and activate data with a goal to improve efficiency as well as patient outcomes. Care teams are also redefining how they operate in a new ecosystem of collaboration. We will continue to see complications in the delivery process because the healthcare industry needs to be transformed in order to realize the best clinical outcomes and financial opportunities by caring as one.
With the decade winding down, we have identified a handful of trends that define this era and are paving the way for future innovation in the healthcare industry as a whole.
A decade of health policymaking
In 2010, we witnessed the enactment of the most significant legislation to impact health coverage in a generation. Throughout the decade, cost management was among the top priorities, resulting in shifts not only in the utilization and the quality, but also in the site of care. These adjustments prompted an increase in the use of ambulatory care, along with the creation of new partnerships and new players in the retail care delivery space.
We also saw an unprecedented focus on prevention and wellness, as well as driving exponential growth in the ways in which chronic care is delivered for the aging population. The rise of high-deductible health plans secured the consumer in the payer seat and drove the need for an increasingly patient-centered care model. Meanwhile, healthcare providers found themselves becoming belabored by the process of catering to administrative needs while sacrificing certain aspects of patient care, such as autonomy and time.
The evolution of alternative payment models
Quality improvement and cost reduction efforts have been around for a while. But until 2010, the U.S. healthcare industry hadn’t really put pen to paper to spell out how providers were to reach a higher quality of care and simultaneously achieve lower costs.
The Centers for Medicare & Medicaid Services (CMS) continued to push for a transition to risk value-based payment methodologies. Alternative payment models (APMs) designed to focus the healthcare system to incentivize quality care delivered with efficiency. The new models tie provider reimbursement to the value of care, meaning providers are remunerated based on their patient outcomes and/or containment of costs. Some reports actively support the cause these models are trying to achieve. Catalyst for Payment Reform recently reported1 that while 53 percent of commercial healthcare payments were tied to value by 2017, care quality improvements and cost reductions were modest. These findings, along with some other data points, indicate that a new era of value-based care has arrived, and it’s going to stay.
The growing importance of social determinants of health
Over this period, stakeholders have realized that success in the value-based ecosystem cannot be achieved based solely on clinical insights. According to one study, clinical care accounts for only 20% of the health outcomes of patients, while health behaviors, social and economic factors, and the physical environment combined add up to influence the remaining 80%.2 Healthy People 2020, a science-based, 10-year national objective for improving the health of all Americans, highlights the importance of addressing the social determinants of health by “creating social and physical environments that promote good health for all” as one of its four overarching goals for the decade.3
Although multiple pieces of research demonstrate that social determinants may substantially contribute to or detract from a person’s health status and well-being, the major problem is still one of resources, considering how to address these complex challenges, and which stakeholder is the best-positioned to do so in a clinical environment.
“At least 25 cents on every dollar spent on healthcare is spent on the treatment of diseases that result from potentially changeable behavior.”4
Data is the key to success and the healthcare platform is the way forward
Data is at the center of the transition to a modern digital health future. Healthcare providers and payers transitioning to more collaborative digital care delivery models are increasingly realizing the need for a new data architecture to support the inherent demands of their move to value-based care.
Foundational to this effort is having a healthcare platform that can transform and unify data from across the healthcare continuum. It must be able to carry the healthcare ecosystem through a new generation of real-time insights and adaptive workflows. These, in turn, must support the operation of varied clinical models, care settings, and administrative drivers, all focused on one goal: the delivery of patient-centered care.
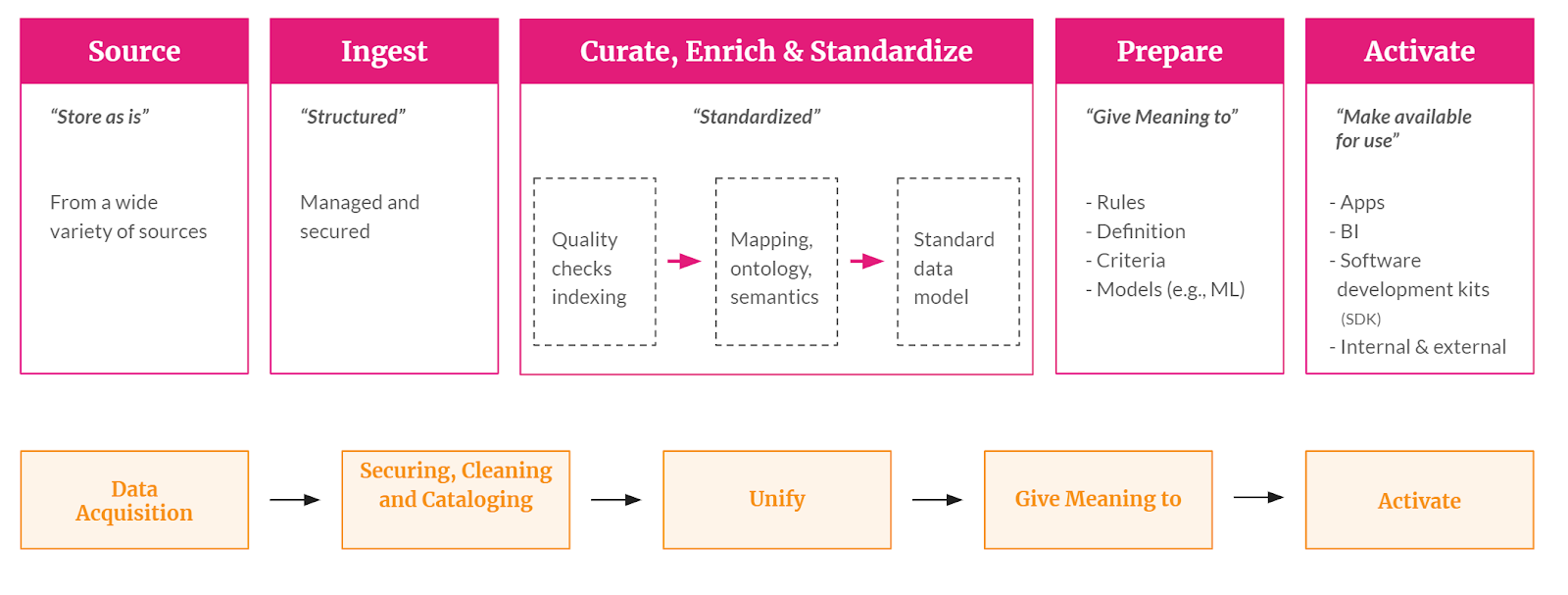
While the term “platform” is used in a variety of ways in different industries, the healthcare data platform collects, stores, enriches, structures, and provides meaning to data collected from across the patient, provider, payer, and community landscape. This platform then analyzes and contextualizes information according to healthcare-specific needs to support a variety of uses and innovations.
Functions of the Healthcare Data Platform
Risk is going to increase and we need to “care as one”
“Risk” was the buzzword for healthcare quality and safety in 2018, as the CMS strongly pushed its value-based payment agenda. The CMS spent the better part of that year strongly supporting the transition to value-based payment. In the midst of this transformation, the CMS has made it clear that its energy is behind alternative payment models that feature downside risk for providers and that the days of one-sided risk are numbered. The confirmation of a new HHS secretary at the start of 2018 signaled the shift. The backing of risk-based payment has rippled beyond the CMS authority, and the industry as a whole is moving toward value-based payment. Moving toward a focus on risk in some form or another—upside, downside, both sides, pay for performance—all of this has definitely become a reality..
For these arrangements to succeed, there is an urgent need to organize healthcare information and make it more accessible to enhance the coordination of patient care while reducing costs - data ingestion, integration, aggregation, and analyses. It's all about taking in the data and placing it in the right context with meaning for every care team member.
Operating on a common platform with a unified patient record will naturally drive providers and care teams onto the same page with a focus on the patient and aligning care as one. Healthcare interfaces are needed that allow the collection of data from the full range of a patient’s healthcare experiences to provide that comprehensive view of the patient for all of the healthcare team. The beauty of such a unified patient record is that data from across the healthcare experiences are joined together to provide a complete view of the patient.
In summary, increasing pressure from employers, payers and the government will drive the movement toward two-sided risk arrangements. Additionally, there has been an uptake in the private sector, with more than half of ACOs bearing the same levels of financial risk in their commercial and Medicaid contracts as in their accountable care contracts with Medicare. Major employers are currently adopting two-sided risk models to control healthcare costs by removing intermediaries and aligning incentives to share savings among employees, providers and the employer.
Rules change. Regulatory environments mold. Yet, the value-based care movement will progress rapidly and globally. And by the looks of the current landscape, the fee-for-service model is squarely in the industry’s rearview mirror.


.png)





.avif)









.svg)
.svg)

.svg)

