The Rise of the AI-Driven Healthcare Analytics Platform: Hype or Reality?


Healthcare executives face an impossible equation daily: improve patient outcomes, reduce costs, satisfy regulators, and keep physicians from burning out—all while navigating fragmented data systems that were never designed to work together.
The State and Science of Value-Based Care 2025 report reveals that "87% of respondents cite financial risk as the top barrier to adoption", even as 64% expect higher revenue from VBC initiatives in 2025 compared to 2024. The disconnect reflects an industry caught between ambitious promises and operational reality.
Meanwhile, research around AI-driven healthcare analytics shows remarkable results:
- Machine learning models can predict high-cost claimants with 91.2% accuracy.
- Medicare Advantage patients in AI-supported Value-Based Care (VBC) programs experience 32.1% fewer inpatient admissions compared to traditional care models.
But after years of technology promises that fell short, healthcare decision-makers are asking the critical question: Is AI genuinely transformative, or just sophisticated vendor hype?
Nothing in healthcare is simple. That's the case here as well.
In this guide, we navigate through the noise to examine real-world evidence, implementation challenges, and the specific factors that separate AI success stories from expensive disappointments.
Why do Healthcare Organizations need a Healthcare Analytics Platform?
Healthcare analytics platforms are centralized systems that collect, process, and analyze data from multiple sources. They process raw, unfiltered EHR data, claims information, laboratory results, imaging, and clinical information to provide actionable insights to improve clinical and operational performance.
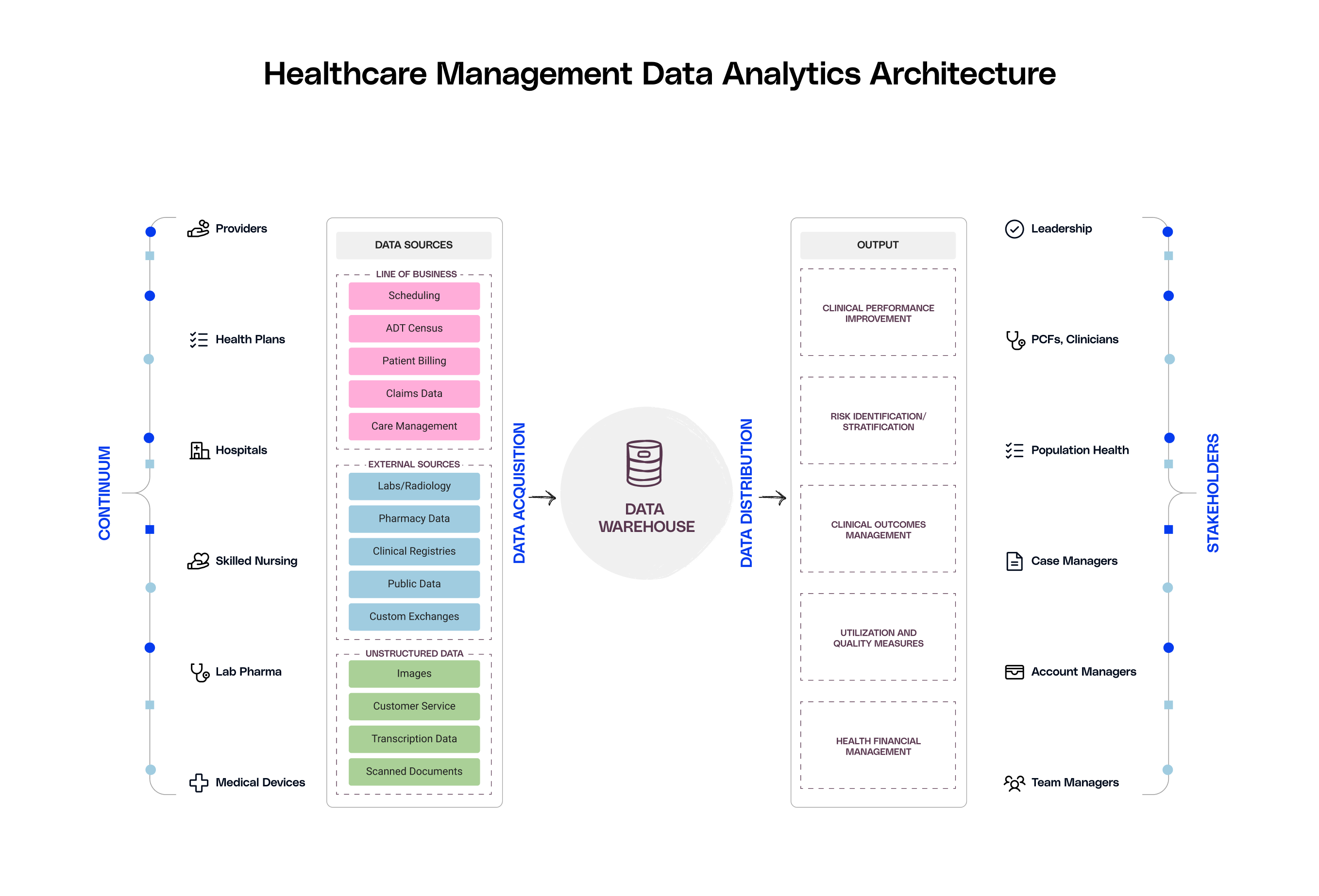
These platforms perform three core functions:
- Data integration across disparate systems
- Advanced analytics including predictive modeling
- Automated reporting for regulatory compliance
They enable population health management, risk stratification, and real-time monitoring of key performance indicators across the entire care delivery spectrum.
By centralising data from multiple sources into one platform, healthcare providers and payers get a comprehensive view of patient populations and organizational performance.
This unified data foundation enables value-based care analytics that identify high-risk patients, predict care gaps, and optimize resource allocation. Consequently, healthcare organizations can transition from reactive interventions to proactive care management, directly supporting VBC contract success.
How is AI Changing Healthcare Analytics?
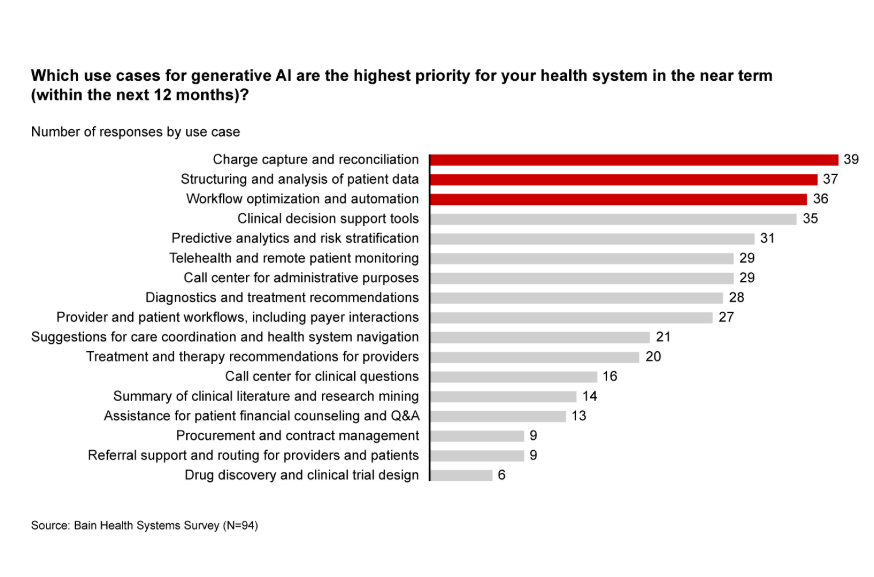
AI is modifying how organizations derive insights from big data by revealing patterns and insights at a speed and magnitude that manual data analysis cannot match. Recent advancements in LLM and natural language processing have brought forward new arenas for healthcare applications.
A study published by an Ivy League University highlights how accurate predictions improved frontline workers’ decision-making, and consequently, had an effect across the organisation.
A leading hospital chain in the United States applied machine learning models to forecast patient outcomes such as discharge dates and ICU transfers. By combining AI predictions with clinicians' assessments, the network observed:
- An increase in patient discharges from 10% to 28.7%
- A 0.67 days reduction in the average length of stay per patient
- Estimated yearly benefits: $55 to $72 million
Traditional Models vs. AI-driven Healthcare Analytics: A Comparison
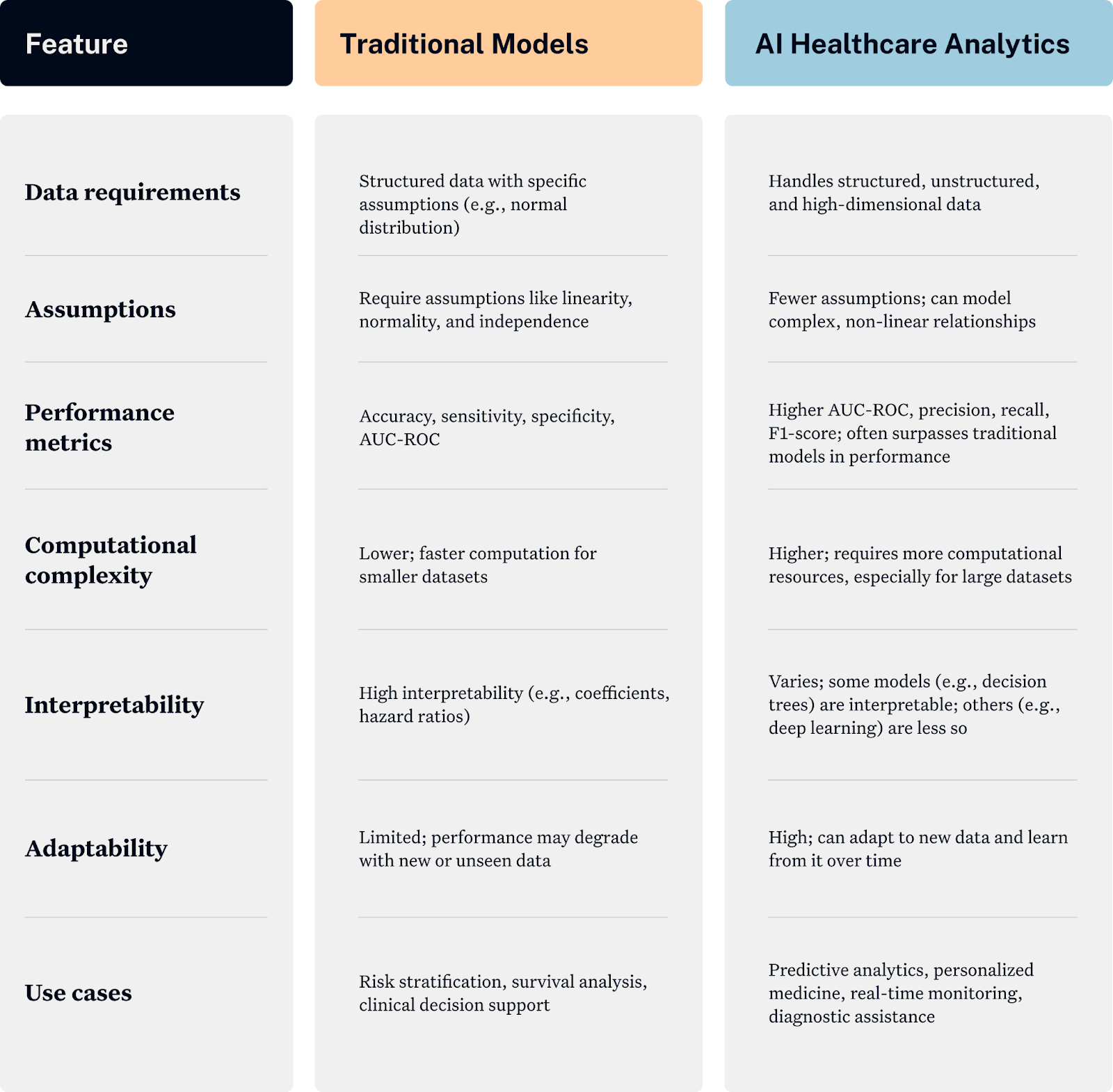
How does AI Help with Population Health Management and Risk Stratification?
When you're supposed to keep the entire patient population healthy while managing costs, traditional methods fall short. AI changes this game entirely by shifting from reactive to proactive care management.
1. Making sense of all your data
AI analytics platforms pull all siloed health data from different sources to create a complete picture of your patient population.
What this looks like in practice:
- Patient data from multiple sources gets combined automatically.
- Social factors like housing instability or food insecurity become part of risk calculations.
- Remote monitoring data from wearables and home devices feeds into real-time assessments.
- Public health databases help identify community-wide trends affecting your patients.
2. Spotting problems before they happen
Instead of waiting for patients to show up in your emergency department, AI helps you identify who's likely to need help next week, next month, or next year.
Predictive capabilities:
- Identifying patients at high risk for readmission within 30 days.
- Spotting early signs of chronic disease progression before symptoms worsen.
- Predicting which patients will likely miss appointments or stop taking medications.
- Forecasting seasonal health trends and resource needs for your community.
3. Getting personal with population health
AI creates individualized risk profiles that help care teams know exactly what each person needs.
Real-world applications:
- Diabetic patients get personalized intervention timing based on their specific risk factors.
- Heart failure patients receive customized monitoring protocols.
- Mental health patients get targeted outreach when data suggests they're struggling.
- Preventive care reminders are timed based on individual risk patterns.
4. Smart Resource Allocation
When you know who needs help most urgently, you can use your limited resources where they'll have the biggest impact.
How organizations are using this:
- Prioritizing high-risk patients for care management programs.
- Allocating case managers based on predicted patient needs.
- Planning staffing levels based on forecasted patient volumes.
- Targeting screening programs to populations most likely to benefit.
5. Risk stratification
Traditional risk scoring often misses the mark because it relies on limited data points. AI-powered risk stratification considers hundreds of variables to create much more accurate predictions.
Advanced capabilities include:
- Real-time risk score updates as new information becomes available.
- Multi-factor analysis that includes clinical, behavioral, and social data.
- Predictive models that learn from your specific patient population.
- Regulatory-compliant scoring that meets CMS and HIPAA requirements.
6. Supporting Value-Based Care Success
AI-driven population health management directly supports your VBC contracts by helping you achieve better outcomes while controlling costs.
VBC-specific benefits:
- Early identification of patients who could become high-cost cases.
- Proactive interventions that prevent expensive healthcare emergencies.
- Better quality measure performance through targeted care management.
- Documentation and reporting that supports shared savings calculations.
Improved Outcomes in Healthcare Organizations Using AI in Data Analytics
While many healthcare executives remain skeptical about AI advancements, many organizations are already seeing measurable improvements that directly impact their bottom line and patient outcomes.
Case Study 1: Children's Health Alliance
The value-based care program at Children's Health Alliance saw an increase in efficiency with AI integration. They were able to reduce administrative overhead by 30% and improve pediatric care coordination. Innovaccer's proprietary healthcare AI integrated social determinants to identify at-risk children before health issues escalate, preventing costly emergency interventions.
Case Study 2: Cleveland Clinic
According to a study conducted by the Cleveland Clinic, their in-house AI-driven risk stratification platform reduced 30-day readmissions by 31%. The predictive model analyzed over 100 patient variables before discharge.
Result? Improved patient satisfaction scores and $2.8 million in cost savings annually.
What are the Challenges of Adopting AI in Healthcare Analytics?
While the benefits are commendable, like any invention, AI in healthcare comes with its own set of challenges, including:
- Data fragmentation and integration: Medical data is siloed across systems (e.g., PACS, EHRs), requiring extensive integration efforts.
- Regulatory constraints: HIPAA and similar regulations limit real-time access to patient data, impacting AI model training and accuracy.
- Clinical adoption barriers: Physician skepticism towards "black box" models demands explainability frameworks, which many platforms lack.
- Operational challenges: Payer representatives often manage overwhelming workloads, with one nurse typically supporting 50 adjusters.
- Technical complexity: Integration with legacy systems poses significant challenges due to incompatibilities and outdated infrastructure.
- Ethical and legal considerations: Ensuring fairness and mitigating bias in AI algorithms is crucial to avoid disparities in healthcare outcomes.

The Final Verdict: Is AI-Driven Healthcare Analytics Platform a Hype or the New Reality?
The evidence supports reality over hype, but with critical distinctions. Healthcare organizations are achieving measurable improvements in patient outcomes, operational efficiency, and financial performance through strategic AI implementation.
However, vendor promises often exceed current capabilities. Experimental features may not be ready for critical healthcare workflows.
So, it is important to set realistic expectations. Start by evaluating your environment and identifying high-impact use cases for AI implementation, and scale slowly. When done right, the benefits far outweigh implementation challenges.

.png)





.png)









.svg)
.svg)

.svg)

