SPOTLIGHT
Empowering health plans to improve member outcomes through value-based pharmacy programs
EmblemHealth, one of the nation's largest nonprofit health insurers, partnered with Innovaccer to launch New York's first pharmacy value-based arrangement focused on improving health outcomes for members with diabetes and hypertension.
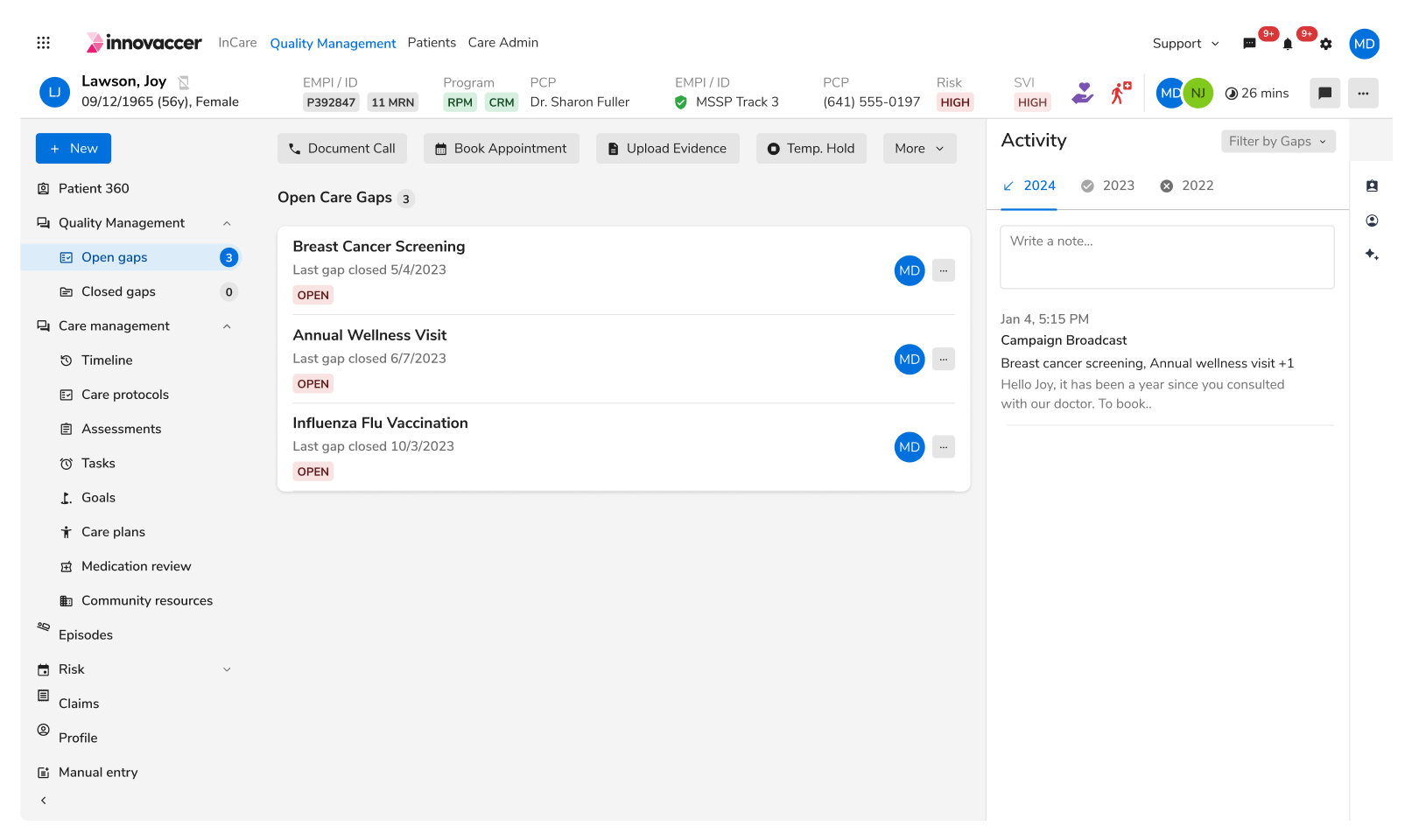
INNOVACCER SERVES EMBLEMHEALTH BY:
Building a unified data foundation to power pharmacy quality programs and care management initiatives that connect pharmacies, providers, and care teams in delivering coordinated, whole-person care.
Augmenting and automating pharmacy engagement, quality reporting, and care team workflows to enable timely interventions and close critical care gaps for chronic conditions like diabetes and hypertension.
Why did Emblem Health choose PQS by Innovaccer?








.avif)





.png)