Prospective vs. Retrospective Risk Adjustment: Which One Yields Better ROI?

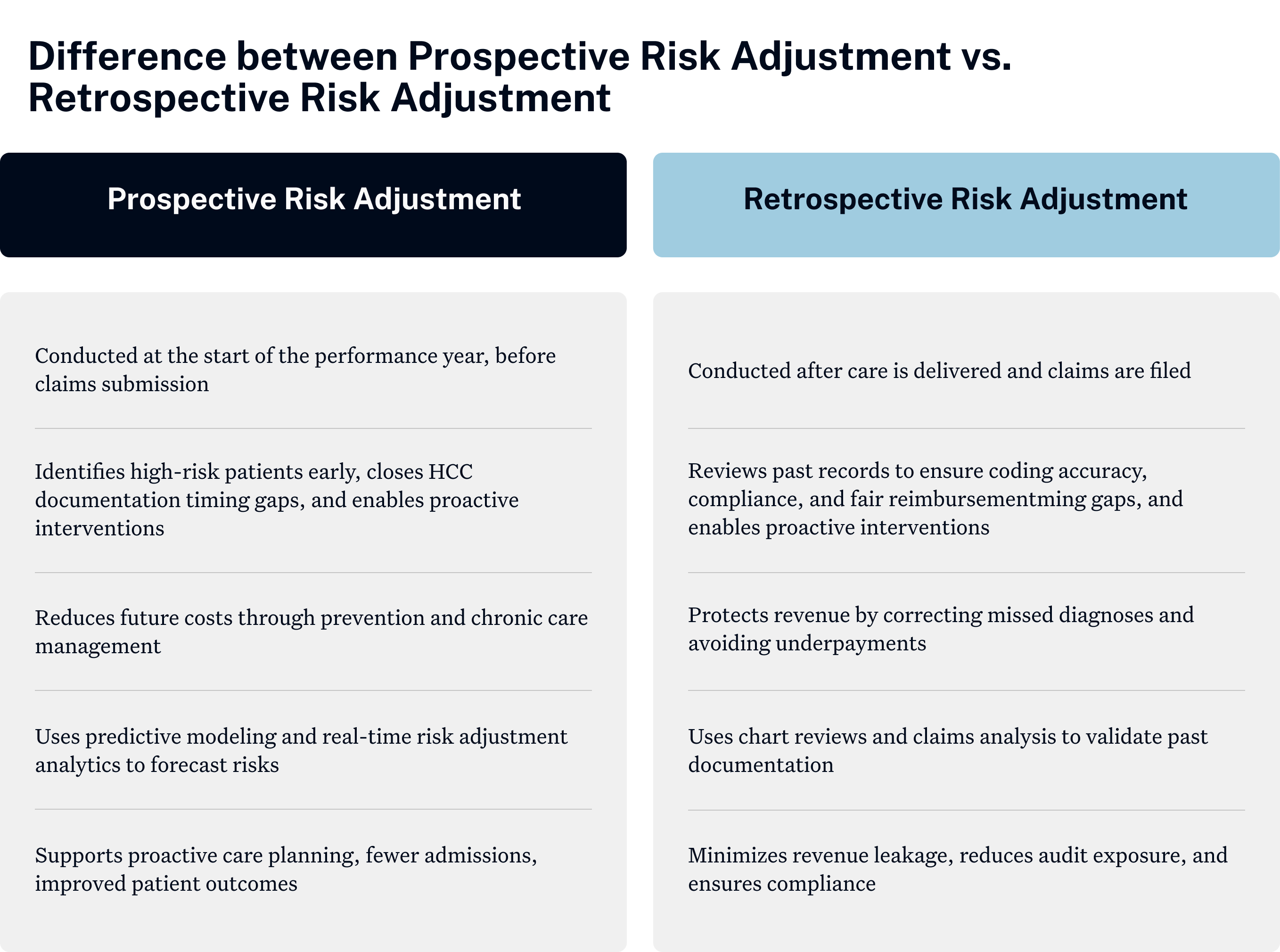
For providers, risk adjustment serves as the backbone of value-based care by ensuring fair reimbursement that accurately reflects the true complexity of the patients they manage. While prospective risk adjustment allows providers to identify high-risk patients early and plan proactive interventions, retrospective risk adjustment reviews past documentation to make sure coding is accurate and payments are correct.
But, providers often wonder: which approach creates more value, or is a hybrid strategy the smarter path? This blog outlines the difference between prospective risk adjustment and retrospective risk adjustment, discusses how they affect ROI, and allows providers to evaluate the ideal strategy for them.
What is Prospective Risk Adjustment?
Prospective risk adjustment empowers providers to anticipate patient risks and address them before claims are filed. By leveraging real-time clinical data and predictive analytics, providers can spot gaps in Hierarchical Condition Category (HCC) coding. They can also preemptively identify patients who can develop complications and intervene promptly with proper care. This not only strengthens documentation accuracy but also reduces audit risks.
For example, consider a diabetic patient who develops early signs of potential condition(s) during his wellness exam. By applying prospective risk adjustment, the clinician is able to accurately document the underlying heart disease, close care gaps, and direct the patient into a cardiac management program.
Employing proactive risk adjustment here will not only prevent any future hospitalizations but also enhance the patient’s long-term health.
What is Retrospective Risk Adjustment?
Retrospective risk adjustment reviews patient records and insurance claims after treatment to ensure all health conditions are properly documented and coded. Unlike prospective methods, which identify risks in advance, retrospective risk adjustment validates documentation from past encounters in order to close documentation and coding gaps, rectify missed diagnoses, or align reimbursement with the true complexity of the patients treated.
For instance, if a patient was hospitalized for heart failure, but their medical record does not reflect their relevant chronic kidney disease, a retrospective review will identify and code this condition. This ensures that the provider receives proper reimbursement and reduces revenue leakage.

Difference between Prospective Risk Adjustment vs. Retrospective Risk Adjustment
Why Prospective Models Are Gaining Traction
Healthcare organizations are now prioritizing prospective risk adjustment for several compelling reasons:
- Closing HCC Documentation Timing Gaps: By integrating into real-time encounters, prospective risk adjustment enables physicians to capture chronic conditions accurately and on time. This prevents missed coding opportunities and ensures complete documentation during the current care year, rather than depending on retrospective corrections later on.
- Utilizing Risk Adjustment Analytics: Advanced predictive tools reasonably enable providers to pinpoint at-risk patients before they encounter complications. By combining data analytics with data-derived clinical insights, providers can rapidly identify and prioritize interventions for at-risk populations. This results in improved care quality and outcomes.
- Achieving Measurable Risk Adjustment ROI: Proactive care through prospective models produces measurable financial and clinical improvements. They have been shown to reduce ER visits and hospital readmissions. This influences provider performance, allowing for fair and sustainable reimbursements.
Also read: Top 10 Leading Healthcare Risk Adjustment Software
Risk Adjustment ROI: What Really Moves the Needle?
The real ROI in risk adjustment isn't solely based on prospective or retrospective models, but rather on a set of factors that determine how effectively a provider captures risks and improves care delivery. These are:
- Accuracy of HCC Documentation: Accurate Hierarchical Condition Category (HCC) documentation is the foundation of risk adjustment ROI, as incorrect coding exposes providers to revenue loss, underpayments, and audit risk. Completed and timely documentation allows patient complexity to be fully recognized, driving fair reimbursements.
- Risk Adjustment Timing: The timing of risk adjustment will have an impact on the ROI. If risk adjustment is done prospectively, it will allow providers to identify high-risk patients earlier and manage conditions proactively. This will reduce the possibility of hospitalizations and increase outcomes.
If it is performed retrospectively, it aids in ensuring reimbursement is accurate and compliant. By reviewing past records, a retrospective risk adjustment may establish if the documentation was valid or, in some circumstances, acceptable. But it does nothing for costs that have already been incurred. In the end, a hybrid approach will often yield the best ROI.
- Physician Engagement and Training: Return on investment (ROI) is compromised even with advanced technology when clinicians are not aligned. Training physicians on best practices for documentation and coding accuracy allows for more accurate patient records. If physicians are engaged, organizations will see better coding accuracy and higher reimbursement overall.
- Compliance and Audit Readiness: ROI also relies on maintaining robust compliance practices. Retrospective review on a regular basis and audit readiness can minimize penalties and protect an organization's financial performance. Having audit-ready documentation protects providers from regulatory risks while also protecting revenue.
How Analytics Drive Better Decisions
Risk Adjustment Analytics is critical in improving the delivery of care and financial performance. Through predictive modeling, dashboards, and AI-oriented recommendations, analytics enables providers to:
- Identify patient risk early: Analytics allows organizations to recognize high-risk populations and intervene before complications worsen.
- Close HCC Documentation timing gaps: Automated alerts during a patient’s visit allow the provider to capture chronic conditions accurately within the performance year.
- Enhance chart review processes: AI-based solutions reduce the number of manual errors, increase coding precision, and reinforce compliance.
- Track Risk Adjustment ROI: analytics connects proactive interventions with measurable outcomes, such as a reduction in ER visits, such as a reduction in ER visits and improvement in quality scores.
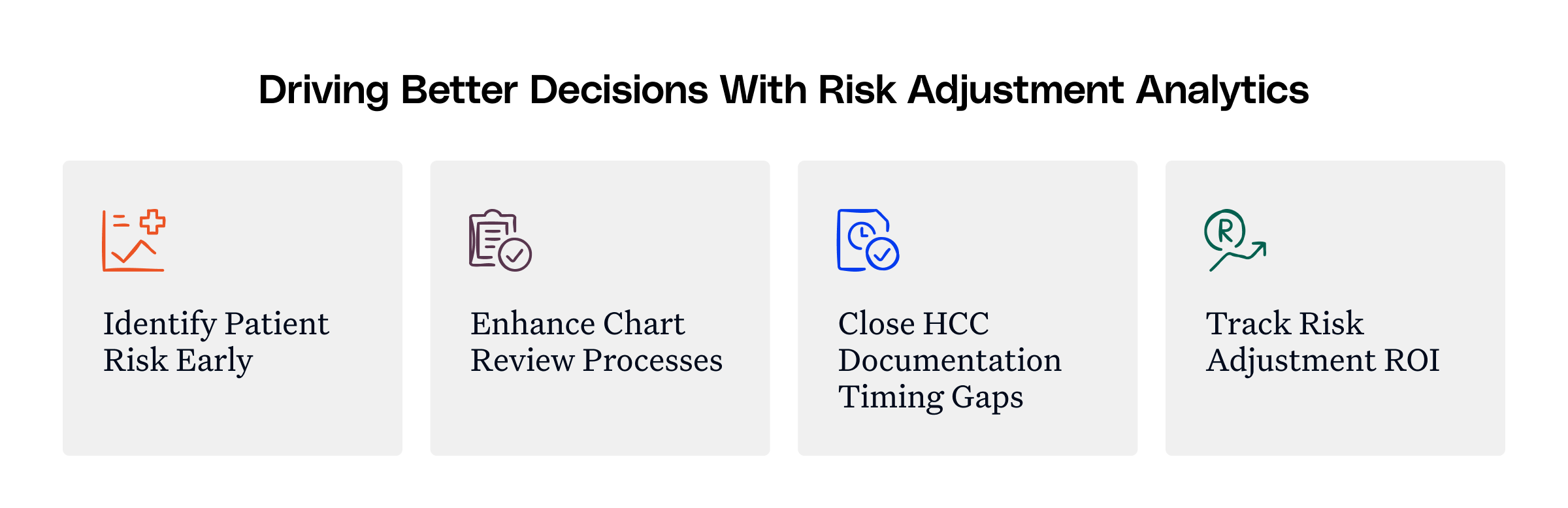
By embedding analytics into both prospective and retrospective workflows, such as value-based care contracts, providers make smarter, data-driven decisions that maximize ROI.
Also read: Built for Providers: How AI is Making Risk Adjustment Work at the Point-of-Care
Best Practices for Blending Both Models
While prospective and retrospective approaches offer unique advantages, the most effective strategy often comes from blending both. A hybrid model ensures that providers not only capture patient complexity in real time but also safeguard revenue through post-encounter validation. Best practices include:
- Create a compliance-first culture: Have documentation prepared to back both future and retrospective workflows for audit readiness.
- Continuously calculate ROI: Monitor clinical results and overall financial performance (as needed) to refine strategies and enhance success over the long term.
- Train clinicians: Train clinicians on accurate HCC documentation as well as how risk adjustment may influence both care and payments.
- Employ advanced risk adjustment analytics: Combine predictive modeling with retrospective claims analysis to gain a full picture of patients’ risk profiles.
How Innovaccer Supports Risk Adjustment
Innovaccer’s AI-powered risk adjustment platform unifies prospective and retrospective workflows on a single data layer, helping providers and payers capture risk more accurately and efficiently. With seamless EHR integration, real-time gap notifications, and direct write-back, providers can document conditions during patient encounters without added burden.
Powered by advanced NLP and predictive analytics, Innovaccer surfaces suspected conditions, closes documentation gaps, and drives up to 30% improvement in coding accuracy and 20% higher RAF scores. The result: reduced administrative costs, stronger compliance, and risk adjustment that becomes a driver of better outcomes and measurable ROI.
Turning Insight into Action
Risk adjustment is no longer about just checking boxes but about driving smarter decisions at the point of care while protecting revenue downstream. Providers who only choose to rely on retrospective reviews risk falling behind in both compliance and quality.
The way forward is clear: adopt a hybrid, AI-powered strategy. By embedding real-time analytics into everyday workflows and reinforcing it with retrospective validation, organizations can reduce missed opportunities, safeguard revenue, and deliver measurable improvements in patient health.
Want to see how AI-driven risk adjustment can improve care delivery while increasing ROI? Connect now.

.png)





.png)









.svg)
.svg)

.svg)

