7 Challenges in Patient Summarization & How AI Eases the Load

Patient summaries are meant to enable healthcare providers to understand a patient’s story in a quick and reliable way - what’s happening, what’s been done, what needs attention. However, creating and reviewing patient summaries is one of the most invisible burdens in healthcare, triggering chaos rather than providing clarity.
Artificial intelligence (AI) is reshaping the patient history summarization process with the help of practical tools addressing real provider pain points. Let’s explore what makes summarizing patient histories so painful for healthcare professionals and how AI is starting to ease their load.
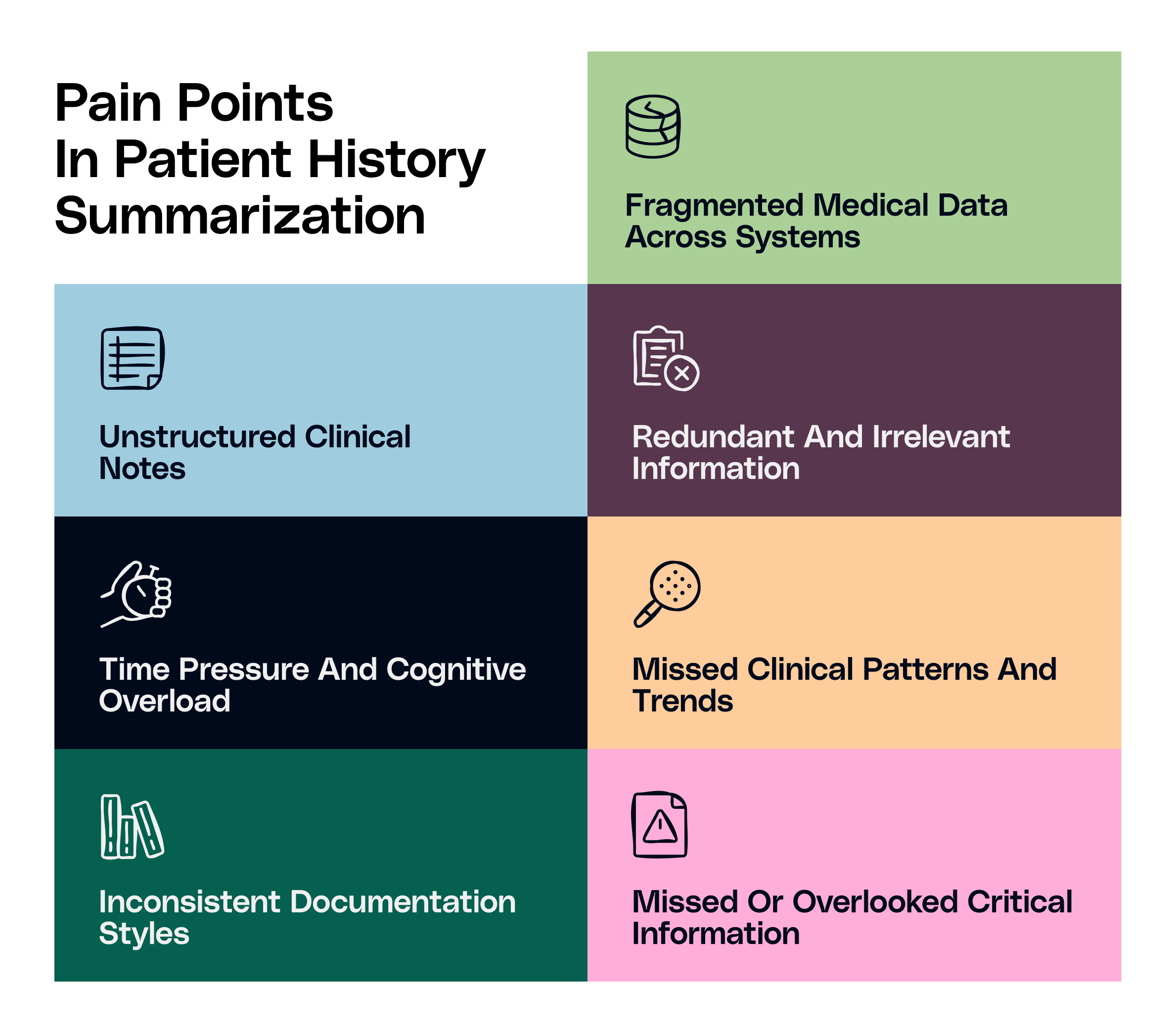
1. Fragmented Medical Data Across Systems | Missing Interoperability
One of the biggest challenges in patient histories is the existence of healthcare data in vast repositories, lacking interoperability. A patient’s medical records might be available in one system, specialist visits in another, lab results in a third-party clinic, and information on hospital stay in its own portal. Providers are left with connecting everything together to obtain clarity of context, leading to wastage of time, slow decision making, and higher levels of risk.
AI solutions help in connecting the dots and making sense of every siloed data. With the right integrations, AI can extract data from multiple systems to organize it into a clean, chronological view. This enables the providers to have a unified view of the full patient journey in one place.
2. Unstructured Clinical Notes
Clinical notes provide the real story about a patient’s medical condition. However, their free-text nature makes them messy and inconsistent. Providers might also have different styles of accumulating patient notes, with one opting for detailed notes and another jotting down just a few bullet points. The inconsistency complicates extracting important information from the notes.
AI assists in easing the complexity with the help of natural language processing (NLP) abilities. It can read through all those notes, extract key clinical information, and summarize them into structured, digestible segments. It extracts all key information from different data, such as symptoms, diagnosis, medications, and lab results, presenting everything right in front of the physician.
3. Redundant and Irrelevant Information
Electronic Health Records (EHRs) are full of clutter, with irrelevant information and outdated details taking the spotlight away from useful data. The same paragraph of a patient’s history gets copied forward in the summaries across multiple visits. Physicians create extensive discharge summaries containing only a few sentences that actually matter. It slows the entire process of pre-visit and post-visit data accumulation, adding a lot of noise and ignoring relevant information in the summaries.
AI provides appropriate tools to filter this noise by segregating important information from the irrelevant. It ensures the summary includes only what is truly relevant by suppressing duplicate content and deprioritizing non-clinical text. The physicians are then presented with a clean chart, empowering them to focus on meaningful information instead of filtering out the junk.
4. Time Pressure and Cognitive Overload
The time allotted for an average primary care visit is very limited, keeping the care coordination team on their toes to review the patient’s chart, form an assessment, document the visit, order labs or any tests, and coordinate follow-up. In essence, the aim is to make the most of a very packed schedule. Adding to the packed schedules, the EHR interfaces look like spreadsheets instead of clinical tools, increasing the cognitive load on the physicians.
AI patient summaries are built to reduce that load. They highlight the relevant changes since the previous visit, identifying what’s unresolved and what needs immediate attention. The prioritization mechanism provides physicians with not just a recap but an action plan to focus on relevant details and act more confidently.
5. Missed Clinical Patterns and Trends
Physicians face different situations where they’ve spotted minute abnormalities in the patient’s health, but no underlying patterns leading to anything serious. Later, with more time and data, the patterns develop into visible trends, leading to a possibility of deterioration in the patient’s condition. The pattern was always there, however, they couldn’t spot it soon enough.
AI tools help surface those patterns. It can track vast amounts of data, such as labs, vitals, and encounters, to flag meaningful changes over time. It visualizes those clinical patterns to save time and enable earlier intervention and treatment modification by the care team.
6. Inconsistent Documentation Styles
Every provider has a different style for documenting clinical notes, complicating handoffs from one physician to another. Some leverage detailed templates, others type freehand. Some include absolutely necessary details, others include everything. This mismatch in documentation triggers confusion in comprehending patient summaries with utmost clarity, leading to complexity in errors in healthcare documentation and diagnosis detection.
AI standardizes the output by following a consistent format with standardized templates, which are easier to scan, interpret, and trust. They don't get affected by multiple formats followed by different physicians and accumulate every information into an easily readable format. This consistency can make a real difference, especially in transitions of care.
7. Missed or Overlooked Critical Information
Long notes can compel physicians to miss or overlook detections of certain allergies or comorbidities. On the contrary, shorter notes in the form of bullet points don’t portray the entire picture of a patient’s condition. The diagnoses aren’t explicitly documented, they’re implied through medications or previous labs.
AI tools are trained on clinical data, which flags those gaps easily. They are quick to recognize multiple scenarios, such as when some information seems missing, when a medication doesn’t align with a diagnosis, or when documentation is inconsistent. That means safer care, fewer errors, and more peace of mind.
Patient Summaries Shouldn’t Be a Puzzle
Healthcare professionals should not be required to reconstruct a patient’s story from scratch at every visit. They shouldn’t be squinting at timelines, scrolling through pages of notes, or trying to guess what happened at an outside facility. AI provides them with clarity to use their clinical skills better by creating easily readable clinical summaries from the different puzzle pieces of patient data.
The technology is ready. All that’s left for healthcare professionals is to leverage it appropriately. Innovaccer provides different solutions to streamline your patient summary creation. Know more about how they can ease your organization’s pre and post-visit documentation. Book a demo today.


.png)






.avif)









.svg)
.svg)

.svg)

