Introducing 360° Gap Closure: The Ultimate Solution to Payers’ Risk and Quality Challenges

For payers, the real challenge goes beyond just spotting gaps in care and risk documentation; it’s about effectively closing those gaps without overwhelming the team or pushing providers away.
With siloed systems, manual processes, and IT departments stretched thin, both identifying and addressing these issues can become a real hassle. The result? Gaps remain open. Providers experience burnout. Members lose interest. This not only leads to missed quality measures but also affects member care, plan ratings, and reimbursement.
To overcome these barriers, there is an increasing need for an integrated platform that enables seamless quality management, risk adjustment, and care coordination to improve member outcomes and satisfaction.
Innovaccer’s 360° Gap Closure solution simplifies the approach to risk adjustment and quality gap closure for payers. By identifying and addressing gaps across providers, members, and pharmacies, the solution enables a data-driven and comprehensive approach to improving care quality and operational efficiency. It empowers payers to improve risk, quality, care, and value-based care outcomes.
Why Now? The Need Has Never Been Greater
Imagine a health plan member who feels dissatisfied with the fragmented care they are receiving. Appointments are delayed by weeks, critical follow-ups are falling through the cracks, and their health is not improving despite best efforts. These incidents are not isolated but represent critical gaps in care delivery that affect thousands of members.
More often than not, members do not receive personalized care because their providers are overwhelmed with administrative tasks like prior authorizations and risk documentation, leaving them with inadequate time to engage with their patients. This not only contributes to missed preventive screenings and evaluating potentially exacerbating conditions but also delays timely treatments for members.
At the payer level, gaps are even clearer. Payers with manual processes and siloed data systems find it difficult to track care gaps for members and even miss documenting risk adjustment opportunities that further worsen member outcomes by not allowing for triggering referrals to other care programs. As payers’ understaffed IT teams are unable to support the integration of data in real-time, they cannot identify closed care gaps effectively, leading to lost reimbursements and poor member satisfaction.
These interconnected challenges demonstrate that we can no longer rely on traditional gap closure approaches, especially as CMS continues to implement additional rules with raised expectations and providers demand better results at a lower cost. Payers require an integrated data platform that can address these gaps and support providers in meeting evolving member needs.

The Solution: Innovaccer’s 360° Gap Closure
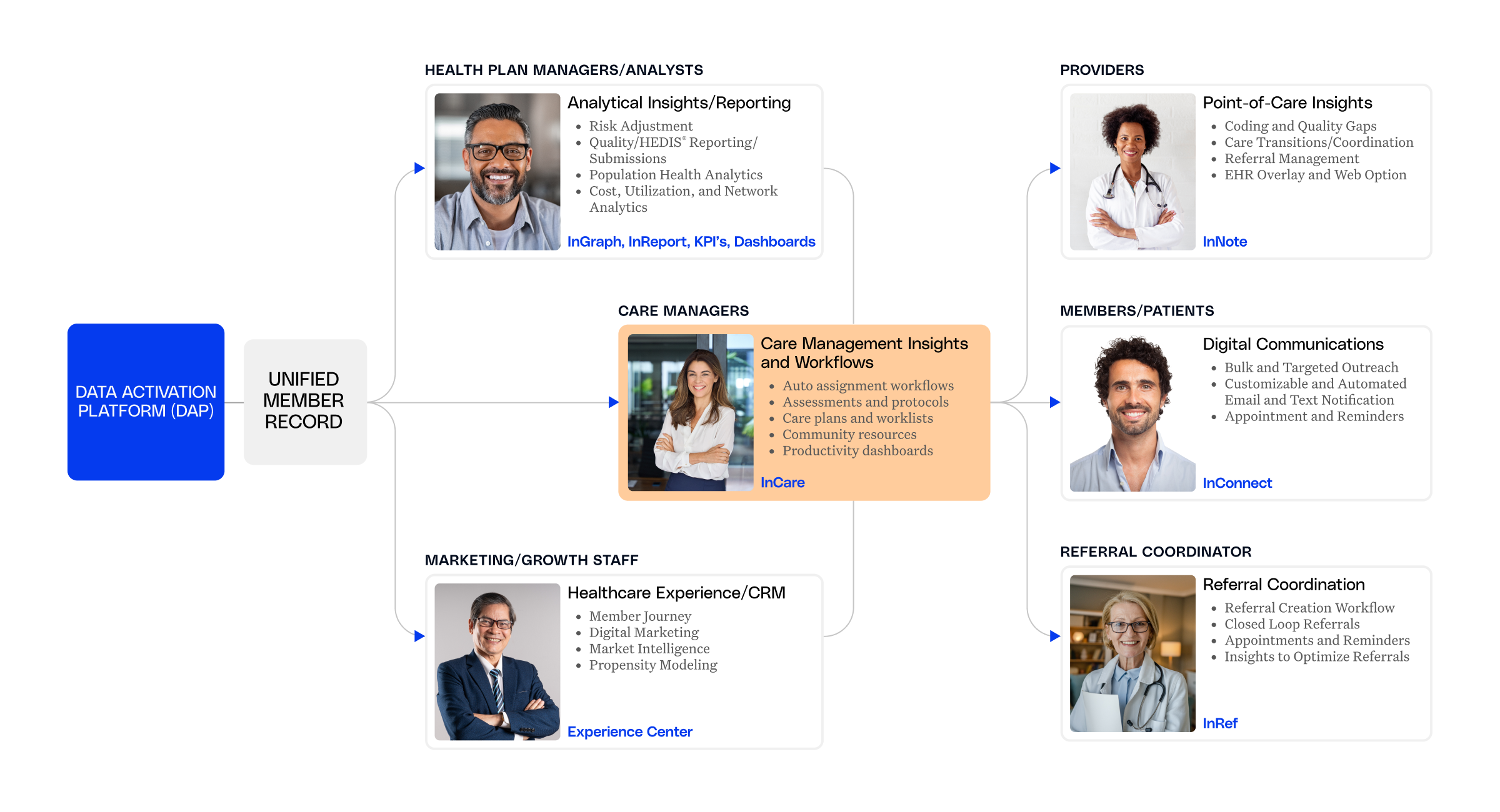
With Innovaccer's 360º Gap Closure, payers can seamlessly address these gaps. This is the first end-to-end, fully integrated solution that empowers payers to identify and close quality and risk gaps within a single platform. By eliminating the need for multiple vendors and disconnected systems, it streamlines care management, risk adjustment, and quality improvement workflows, ultimately enhancing both provider and member experiences.
Through prospective, concurrent, and retrospective reviews, the solution ensures continuous quality improvement with an automated and human-in-the-loop review process. Its automated data governance framework reduces the burden on IT teams significantly and simplifies workflows, improving the experience for risk, quality, and care managers.
Here’s how Innovaccer’s solution is helping payers close risk and quality care gaps and drive value-based care outcomes:
Driving Better Adherence to Medications and Screenings through Pharmacy Partnerships
By partnering with pharmacies, the solution enables payers to increase immunizations, improve adherence to medications, and close care gaps effectively. Through real-time insights and automated reporting, payers can act quickly to deliver timely care. This not only boosts Star ratings but also strengthens relationships with members.
Strengthening Provider Collaboration and Member Engagement with AI
The solution personalizes multi-channel communication (emails, SMS) with members and enhances collaboration with providers through actionable insights. It also makes it easier for providers to work with payers by giving them real-time insights and automating tasks like authorizations. With bi-directional integration with EHRs, providers can close gaps faster, spend less time on paperwork, and focus more on delivering better care.
Also, the presence of a bi-directional query system lets providers resolve documentation issues, if any. This reduces provider abrasion and ensures that records are accurate.
Empowering Members with At-home Care and Early Interventions
The solution enables payers to conveniently order at-home test kits, schedule PCP visits, or even encourage vaccination at pharmacies, all with one-click campaigns. Intelligent reminders and automated follow-ups enhance member participation and increase preventive screening rates. Members are empowered to manage their health, resulting in early risk detection and improved outcomes.
Accelerating Coding Accuracy and Risk Adjustment with AI
The AI-powered 360° Gap Closure solution streamlines chart retrieval, coding, and concurrent reviews. It ensures the accuracy of clinical documentation by reviewing it before, during, and
after a patient’s visit, helping providers capture accurate information in real-time and meet quality standards. The solution also streamlines clinical documentation for quality measures and risk adjustment with the help of AI while still maintaining expert human oversight to ensure documentation accuracy and regulatory compliance.
Impact: Drive Outcomes Without the Extra Cost, or the Stress
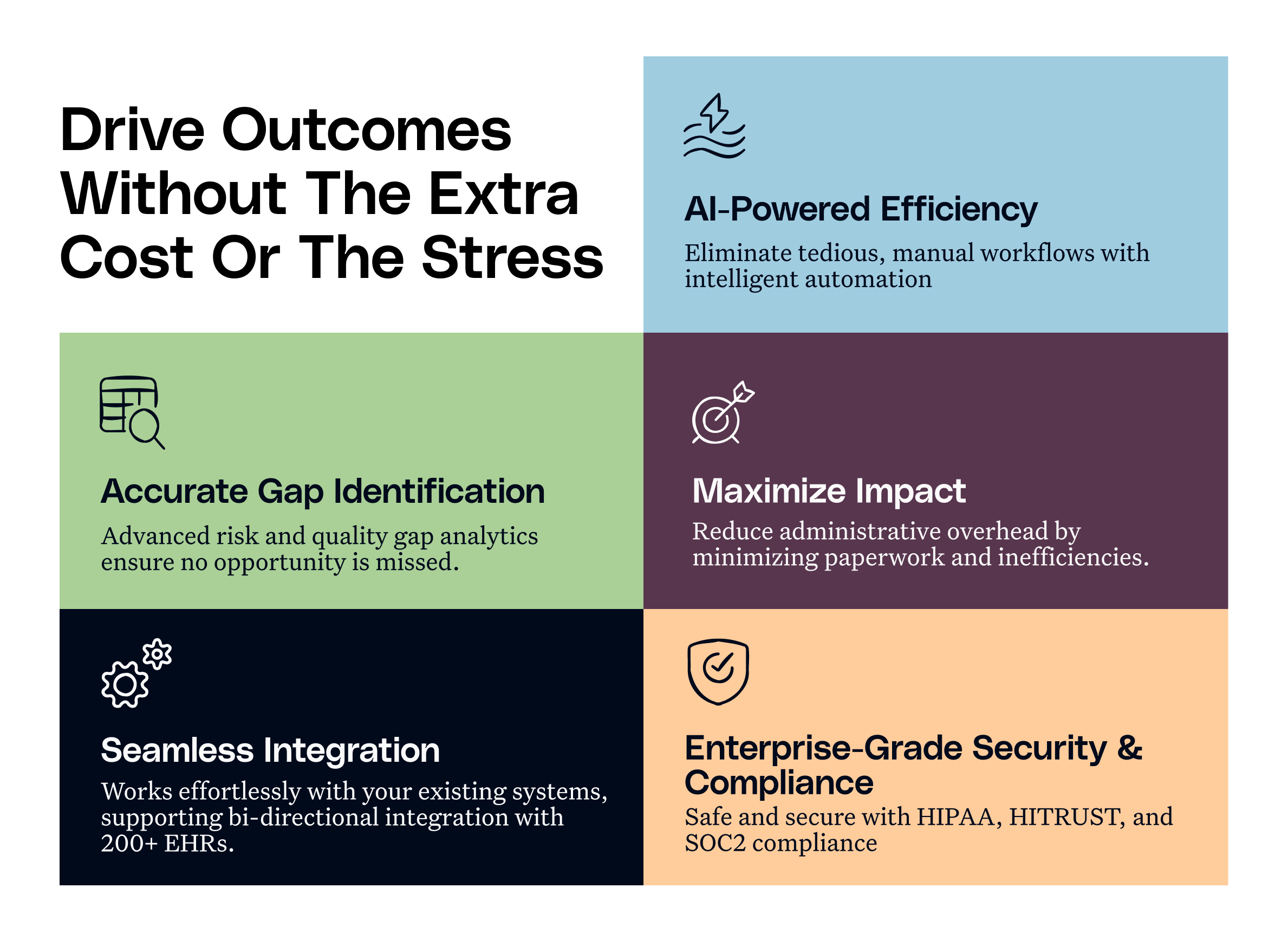
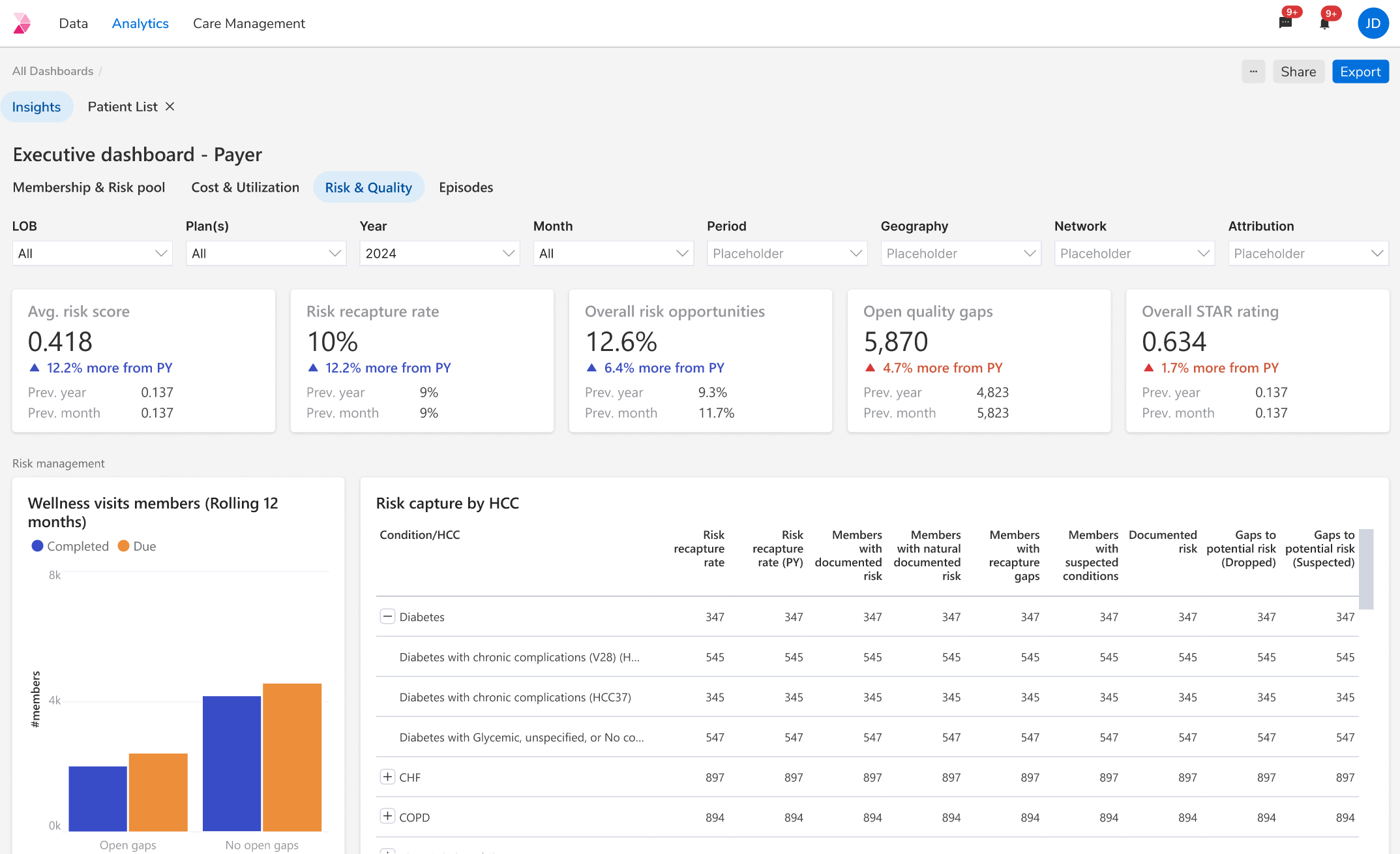
- Accurate gap identification: Payers can leverage advanced analytics to spot monthly quality and risk gaps, ensuring timely and targeted interventions.
- Effortless data management for maximum impact: The solution automates data template loading, enables bi-directional EHR integration, and routes campaign data to the right dashboards, reducing the burden on IT teams significantly and simplifying claims processing.
- Streamlined workflows, powered by Artificial Intelligence: The solution enables intelligent automation, which removes the need for manual and error-prone processes and operational overhead so that teams can focus on what matters most-delivering care.
- Connected systems for delivering care seamlessly: The solution connects to over 200 EHRs effortlessly through bi-directional data exchange, while requiring minimal IT effort. It ensures that real-time and accurate information is shared where needed most.
- Enterprise-grade security and compliance: Payers can rest assured as the solution is compliant with HIPAA, HITRUST, and SOC 2 standards, and NCQA DAV certification, protecting patient information while meeting the highest industry benchmarks.
Overall, Innovaccer’s solution helps payers improve care quality, streamline operations, cut IT and record retrieval costs, reduce provider friction, and achieve better health outcomes for members while driving value-based care success.
Take Charge of Your Gap Closure Strategy
With CMS regulations tightening up, it’s time to reinvent your approach to care. Innovaccer’s 360° Gap Closure platform gives you the power to act quickly and effectively across every touchpoint. Don’t just report outcomes, but rather take control and drive results.
Take the first step toward a risk and quality process that’s smarter and seamless for your team. Book a demo


.png)






.avif)









.svg)
.svg)

.svg)

