Gearing Up for CMS TEAM Model: A Comprehensive Guide to Healthcare's Next Evolution

The Centers for Medicare & Medicaid Services (CMS) continue to drive innovation in healthcare, ensuring quality, efficiency, and value-based outcomes. To further create impact, they recently introduced TEAM (Transforming Episode Accountability Model)- a groundbreaking initiative aimed at redefining care delivery and payment structures. As healthcare organizations prepare for the transition to TEAM, understanding the intricacies of the TEAM Model is crucial for success.
Let’s break down how the TEAM Model can revolutionize value-based care.
What is TEAM (Transforming Episode Accountability Model)?
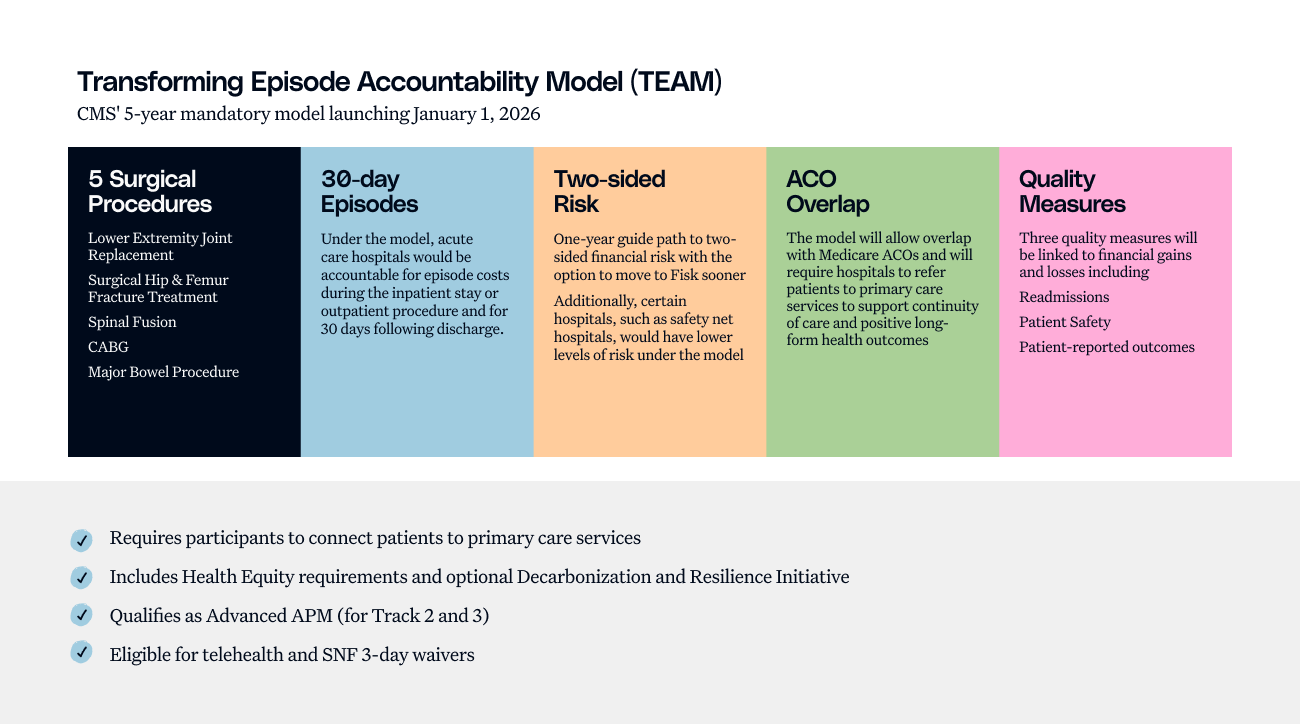
TEAM (Transforming Episode Accountability Model) is an episode-based payment approach that shifts the focus from volume to value, ensuring providers deliver efficient, high-quality care while managing costs effectively.
Particularly designed for hospitals, post-acute care providers, and patients they serve, TEAM builds upon previous bundled payment models but introduces more advanced risk-sharing mechanisms, patient-centered quality measures, and incentives to drive significant improvements in care outcomes and financial sustainability for healthcare organizations.
TEAM is a five-year program that is set to begin on January 1, 2026, and is expected to run through December 31, 2030. Acute care hospitals in specific Core-Based Statistical Areas (CBSAs) across the US are required to participate mandatorily. The way that more than 700 hospitals across the country handle financial management and service delivery will be drastically altered by this episode-based payment model.
Why TEAM? Challenges with Bundled Payments
Before TEAM, CMS experimented with different bundled payment initiatives, starting with the Bundled Payments for Care Improvement (BPCI) model in 2013, and followed by Comprehensive Care for Joint Replacement (CJR) model in 2016.
While these payment systems improved efficiency, they faced significant challenges, including voluntary participation and selective care episodes. Adoption was limited as only two out of nine eligible hospitals opted into programs like CJR, which created uneven participation. High-performing institutions joined in while others avoided complex cases, limiting systemic improvement. Additionally, it was challenging to coordinate care through the 90-day post-hospitalization period.
To address these challenges, CMS designed TEAM as a mandatory model with universal participation and a more manageable 30-day care window, fostering broader transformation.
How TEAM Payments Work?
The TEAM model allows hospitals to share reconciliation payments with doctors and other providers involved in a patient’s treatment. This encourages them to work together to provide high-quality and cost-effective care.
In addition to receiving target costs for certain episodes of care, hospitals will still be able to bill Medicare as usual. Based on three years of baseline data, the target prices have been modified to account for variables such as area and episode complexity.
Hospitals will be evaluated on how well they execute on specific quality metrics and how much they really spend in comparison to the goal price. Medicare will reimburse hospitals if they achieve quality standards and spend less than the target price. But they will have to pay back Medicare if they spend more than the set amount.
.png)
CMS’s Goal with TEAM
Medicare beneficiaries who have specific surgical procedures would have their care coordinated by a few chosen hospitals under the TEAM model, starting at the time of the procedure and continuing for 30 days beyond the patient's discharge. All goods and services rendered during a care episode are the responsibility of the hospital. This guarantees a thorough and well-coordinated method of patient treatment.
“If the planned TEAM is effective,” CMS stated in the proposed regulation, “It may open the door for managing episodes as a standard practice in Traditional Medicare.”
Key Features of TEAM
The TEAM Model enhances care delivery through episode-based payments, risk-sharing, quality incentives, and data-driven decision-making. It encourages broader provider participation to drive better outcomes and cost efficiency. Here are some key features:
- Shorter 30-Day Post-hospitalization Period - Replaces the previous 90-day timeframe, making care management more focused and effective.
- Episodic, Quality-driven Payment Structure - Providers are reimbursed based on comprehensive care episodes and patient outcomes rather than fragmented fee-for-service billing.
- Data-Driven Decision-Making - Enhanced analytics and interoperability will play a significant role in improving care coordination.
- Expanded Provider Participation - The model is expected to be more inclusive, bringing in specialists, hospitals, and post-acute care providers.
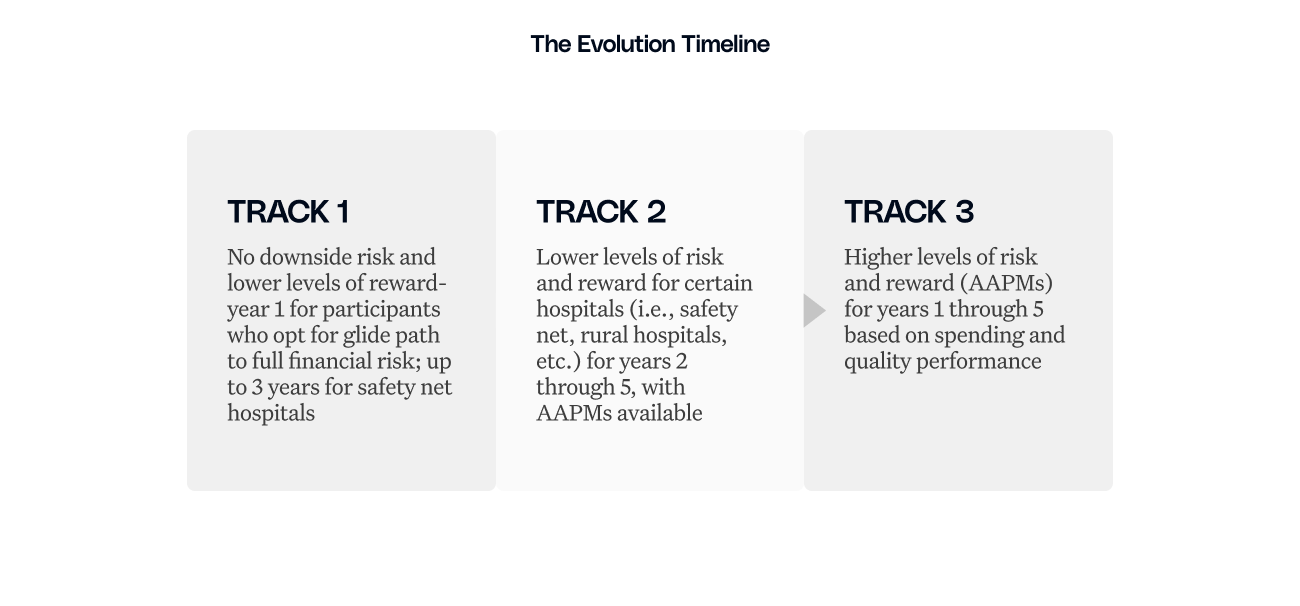
Risk Sharing Mechanisms or the Three-track Participation System: Acute care hospitals accommodating varying risk readiness levels and institutional capacity have to follow the three-track participation system:
Quality Measures for TEAM
The TEAM Model ties hospital reimbursements to both cost efficiency and quality performance. Hospitals must meet specific quality measures to receive additional payments, ensuring patient care remains a priority.
Key Quality Measures in TEAM:
- Spending vs. Target Price - Hospitals are evaluated on whether their actual expenditures fall below predetermined CMS target prices.
- Readmission Rates - Lower readmissions indicate better post-discharge care and care coordination.
- Complication Rates - Hospitals must minimize complications and adverse events within the 30-day episode period.
- Patient Experience & Satisfaction - Measures based on patient surveys assess the quality of care from the patient’s perspective.
- Clinical Best Practices Compliance - Providers must adhere to evidence-based treatment protocols.
Hospitals that meet both cost and quality targets receive additional Medicare payments, while those that exceed spending limits face repayment obligations to CMS. This ensures a balanced focus on cost efficiency and patient outcomes under TEAM.
Importance of TEAM for Healthcare Stakeholders
The success of TEAM depends on collaboration across the healthcare continuum. Post-acute care providers, Accountable Care Organizations (ACOs), and primary care physicians are key stakeholders of the model. Organizations participating in the model face both risks and financial opportunities, as hospitals can earn reimbursement by keeping ideal costs below the target. Nonetheless, if the expense exceeds the target, CMS demands repayment.
- For providers, the 30-day post-hospitalization period creates financial accountability, creating stronger care coordination practices.
- Meanwhile, payers benefit by focusing on cost control and quality outcomes.
- Value-based care organizations gain a complementary framework that strengthens existing quality initiatives through the model's regional average pricing approach and risk adjustment mechanisms.
- ACOs specifically align with TEAM frameworks as they create opportunities for enhanced care coordination and collaborative cost management strategies.
Watch the Webinar: Navigating the New CMS TEAM Bundled Payments Program for 2026
Strategic Implications of TEAM and the Road Ahead
The model introduces both adaptability and accountability challenges for care coordinators. The 30-day post-hospitalization period requires fast-tracked care coordination and advanced healthcare analytics tools to identify high-risk patients.
To address these challenges, TEAM provides financial reasoning for enhanced risk adjustment, cost management, and predictive analytics capabilities. During this 30-day post-hospitalization period, readmission becomes the primary area of focus both for the healthcare facility and the patients. This represents a paradigm shift, where the organizations are not just transforming care expenses but are also redesigning the care transition protocols.
The path to success requires a careful integration of patient care priorities with operational efficiency. Organizations that approach TEAM strategically and invest in care coordination while developing strong analytical capabilities, can transform these post-acute challenges into a catalyst for meaningful improvement.
By partnering with organizations that truly understand the nuances of care coordination hospitals can turn TEAM for meaningful improvement that resonates with patients and providers alike.
How Can Innovaccer Help?
With Innovaccer’s integrated suite of solutions, hospitals can very smoothly navigate through the complexities of the CMS TEAM Model. Organizations can implement Innovaccer’s exceptional VBC solution which includes tools that help streamline financial analytics, contract management, and quality reporting into a single, and unified platform.
The solution's health equity initiatives and other capabilities give organizations the confidence to adapt to the TEAM model. Innovaccer's solution suite enables proactive interventions that reduce readmissions and improve patient outcomes.
Key capabilities of the platform include:
- EHR-agnostic care management workflows with seamless integration into existing hospital systems
- Real-time analytics and performance dashboards to track trending costs and benchmarks
- AI-driven financial analytics for risk adjustment, predictive modeling, and reimbursement optimization
- Automated alerts and patient outreach tools to streamline care transitions and improve engagement
Success with TEAM is not just about compliance; it’s about the smooth transformation. With Innovaccer’s AI-driven platform you can discover a smarter approach to the reimbursement model. Request a demo now!


.png)






.avif)









.svg)
.svg)

.svg)

