AI-Supported Care Management
.png)
.png)
AI-Supported Care Management
.png)
.png)












Raw data is received from source systems and stored in the lake before any processing and interpretation. Your original data is always available to diagnose any issues and enable reprocessing as issues are resolved.
Patient and provider information are aggregated into a single record containing multiple sources of information through Master Data Management functionality, including an Enterprise Master Patient Index, and data curation to remove redundancies. The data at this level is leveraged for application functionality and downstream processing.
The raw data is parsed and codified, then stored in a simple and clean data structure without complex relational features. The data at this level is typed and coded to the UDM’s ontology and ready to be processed into the downstream structures, which are leveraged for applications and analytics.
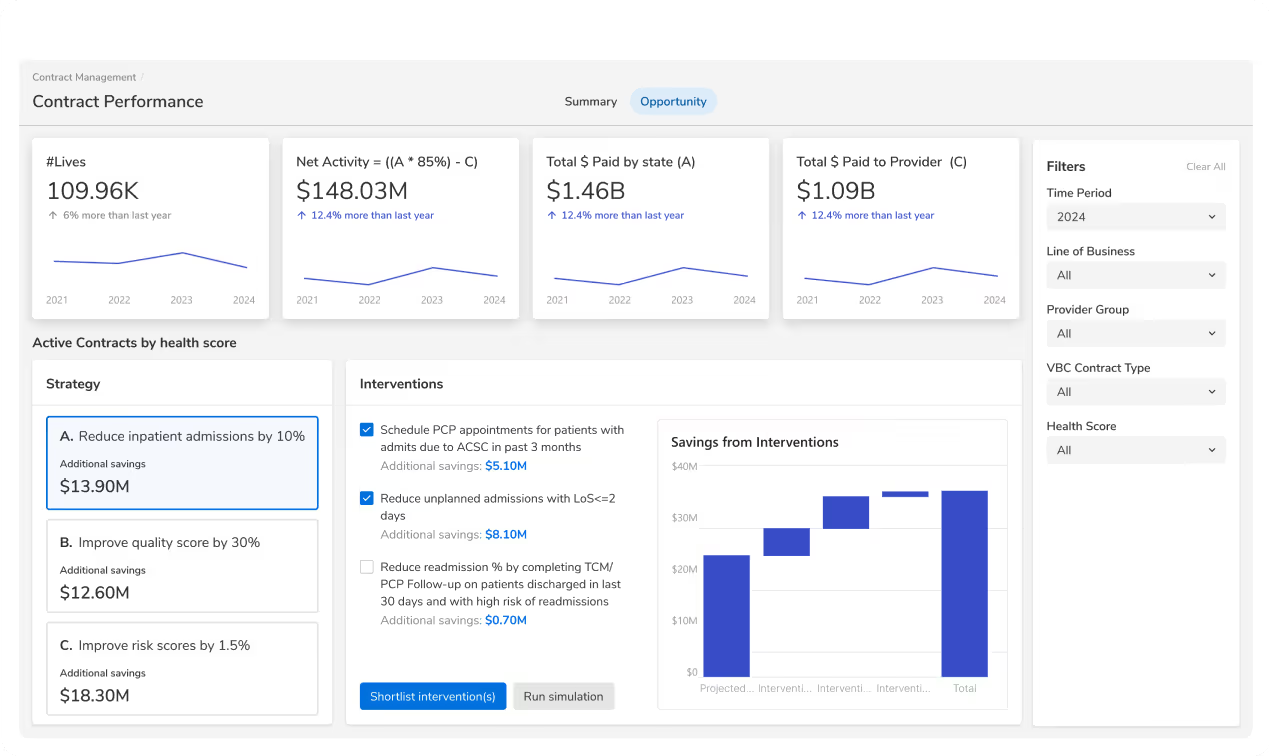
Intelligent algorithms enrich the data the previous stage with deep insights. Out of the box, this includes each patient’s disposition toward quality measures (numerator, denominator, exclusions), risk and social vulnerability profiles, gaps in care, engagement data, next best actions, and more.
Analytics summarize and denormalize the data from Unify and Process stages into a multidimensional data cube structure optimized for analytics, AI, workflows, and additional data visualization use-cases.
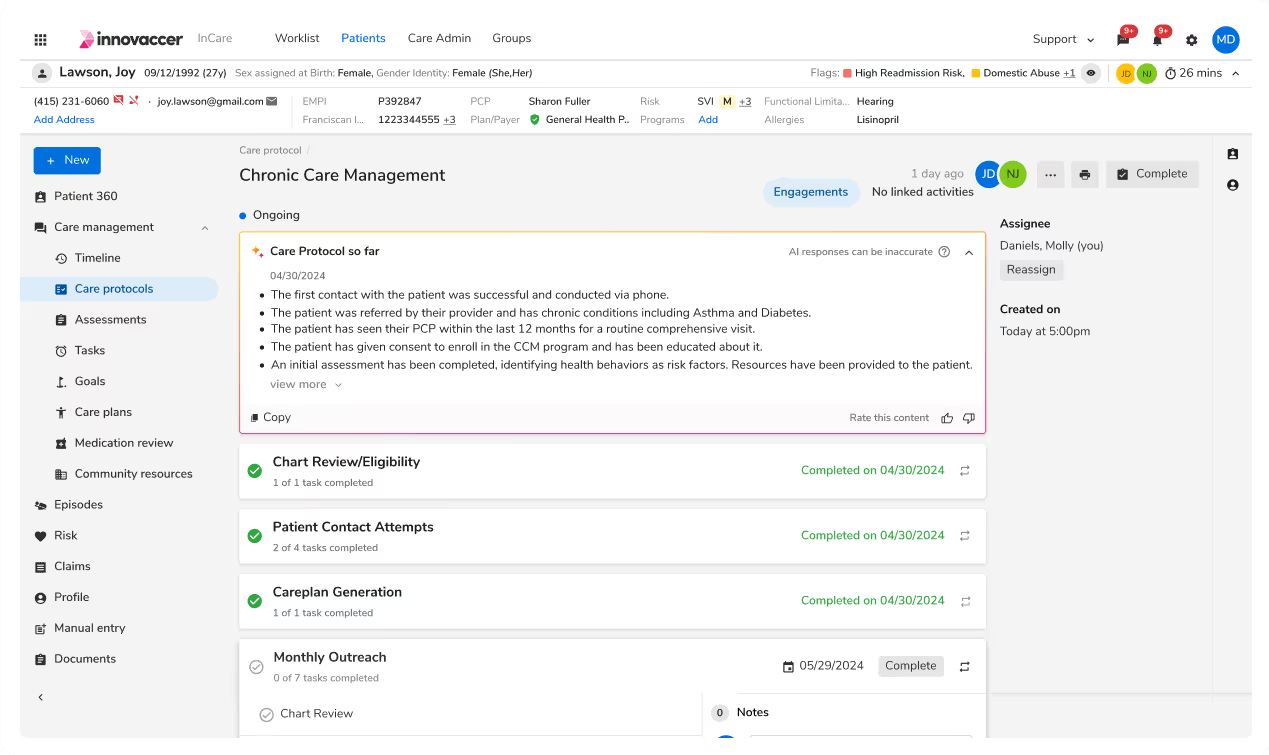
We seamlessly integrate with your EHR, claims database, and other IT systems to ensure care managers have every piece of data at their fingertips.
