Risk Scoring 101: America’s Need to go Beyond Traditional Healthcare

Lidia is a Nebraskan in her mid-thirties, who recently discovered that her body had been predisposed to sickness due to a genetic disorder. One of the genes in her body that’s supposed to fix DNA-copying errors during cell division is not functional, and if the body can’t make up for those minor mistakes, the cells could replicate and snowball into a malignant tumor. Lidia’s PCP and her care team realized Lidia’s health status and were fully aware what it could lead to if ignored. A prepared care team and targeted interventions have empowered Lidia to take full charge of her lifestyle habits to improve her odds.
Risk scores play a vital role in identifying an at-risk patient. But it is more important to identify the type of risk: whether it requires immediate intervention or not.
Why does healthcare need risk scores? Aren’t there enough numbers already?
We hear statements such as—“There’s a 40% chance of gusty and blustery winds today,” “The Yankees have won all of their games this season, so it is highly likely that they would defeat the worst team on the roster,” or “On average, smokers die 10 years earlier than nonsmokers.” These are mere stats, and they can be marvelous, bizarre, and unbelievable- all at once. They strongly influence people’s behavior as they are based on evidence or data findings from years of surveying, studying, and analyzing past trends and occurrences.
We have been predicting future events across a spectrum of domains- from weather, sports, elections, to lifestyle choices and public health. The reason for this incessant collecting, analyzing and predicting future outcomes can be summed up in 3 simple words—forewarned is forearmed.
The current state of risk scores in healthcare
Almost all kinds of care organizations have some risk scoring methodology to target care interventions. Fundamentally, a risk score is a standardized metric for the likelihood of a person encountering an episode. It can predict hospital readmission or even the development of a particular condition. For healthcare payers, risk scores for members are the key metrics to reserve for risk-adjusted payments to Medicare.
Actuarial sciences were where risk scores got their start and are still widely used to help providers and payers anticipate the cost and time of covering different patients. Though extremely useful for population assessment, risk scores aren’t simply designed to consider the risks of individuals. A worsening risk score could perhaps mean that the disease a person has is worsening, or it could mean that the person contracted a new illness, or it could be a combination of the two. In any case, the current methodologies need to provide a complete picture of population health as well. The risk scores are a quantification of patient demographics and prior diagnoses, and they end up being more reactive than predictive.
Why do risk scores of today spell trouble for tomorrow?
Utilization events, clinical details, and lifestyle indicators are used by organizations to chart how these factors influence ultimate outcomes. And finally, they help in developing strategies to keep the population healthy at lower costs.
There could be a number of strategies to manage population health, but there’s no such thing as “one size fits all.” The risk faced by a complicated pregnancy cannot be measured with the same data and algorithms as the risk of a congestive heart failure. No two patients are same. The algorithms and data sets to predict their risk scores shouldn’t be same either.
Moving beyond ‘one-size-fits-all’
With quality, costs, and patient experience taking the center stage in healthcare, care organizations need to stratify patients based on their need for an immediate intervention. The need of the hour is to address high-risk issues that impact large groups of patients and ensure that these needs are met in a timely fashion.
Predictive modeling can proactively identify patients with higher risk, who can later benefit the most from an intervention. Advances in analytics and machine learning have made it possible to use different types of data to develop highly-personalized targeting.
A Success Story
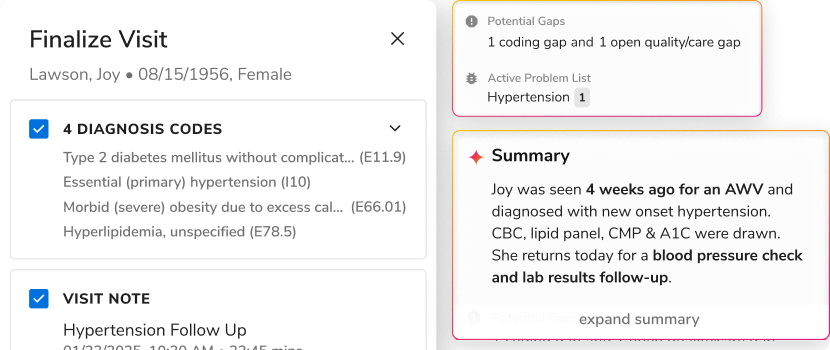
An ACO based out of Midwest America was relying on CMS-HCC risk model to score patients covered by their Medicare contract. Out of all the 90,000 Medicare lives, the ACO was looking to segment the ones with a risk score higher than 1.2. The CMS-HCC scoring revealed that there were 16,000 patients in need of immediate attention. However, the ACO decided to drill deeper into the results, looking for a more accurate analysis and stratification.
The ACO expanded the range of data they were using and incorporated network’s utilization data and SDOH on a single healthcare data platform to enhance risk stratification. This deeper analysis, four times more accurate, revealed that only 3,600 patients were in the need of an intervention as opposed to previously-predicted 16,000. Also, the ACO providers found that out of these 3,600 lives, only 1,700 had visited a hospital at least once. Equipped with this knowledge, the ACO then began planning targeted and accurate care management, ultimately reducing the 30-day readmission in their network by 9.12% and ED visits by 11.37%.
The key- when it comes to finding people “at risk,” the more relevant data we have, the better.
The road ahead
Data is going to play a crucial role in the future of healthcare, but analyzing that data for actionable insights is going to be the key. Today, with the use of data we can tell who needs an intervention, and the possibilities are endless. We can predict the future of patient-centric care, we can tell beforehand who might fall sick and how much can a procedure cost. Healthcare has become advanced enough where we can say that the entire space is proactive. We do not have to wait for a disease, we have to keep everyone healthy because we can.
To learn how actionable risk scores can help you improve outcomes across the care continuum, get a demo.
For more updates, subscribe.
Join us at the 15th Annual World Health Care Congress at The Marriott Wardman Park Hotel, Washington, D.C. from April 29th to May 2nd at booth #507, and learn how Innovaccer’s healthcare data platform can assist you in achieving successful outcomes.

.png)



.png)









.svg)
.svg)

.svg)

