Before You Click “Submit”: 6 Questions to Answer Before Applying to ACCESS

TL;DR
Applications for the CMS ACCESS Model are now open, with an April 1 deadline for Cohort 1. While the application is straightforward, the execution is not.
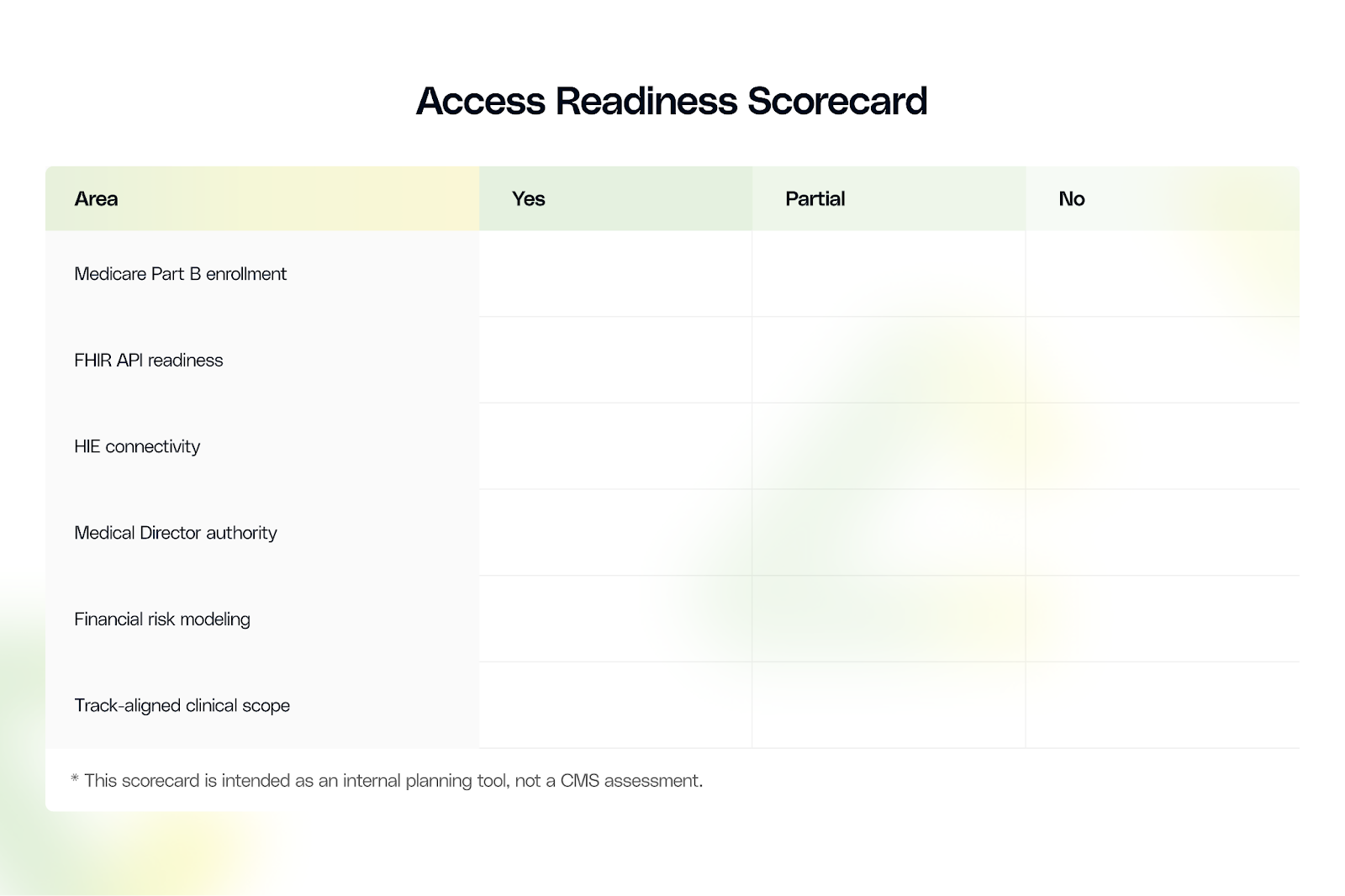
These six questions help determine whether your organization is actually ready to participate in Cohort 1 or whether Cohort 2 is the more realistic and lower-risk path.
Most organizations considering the ACCESS model already understand the strategic importance of the new CMS model. The more immediate risk is applying before foundational requirements are in place.
Designed to operate on real-time data exchange, outcome accountability, and clinical governance, those expectations begin on day one of the performance period. Organizations that apply without readiness will expose themselves to delayed payments, corrective action plans, and downstream compliance risk.
This makes readiness assessment the most important step in the ACCESS decision process. The six questions below are designed to surface execution risk early, while there is still time to adjust course.
Q1: Do You Have Medicare Part B Enrollment Today?
Each ACCESS Participant must be identified by a single Medicare Part B enrolled Taxpayer Identification Number and be eligible to bill under the Medicare Physician Fee Schedule. Organizations that are not currently enrolled must complete Medicare enrollment before participation.
CMS has stated that applications will not be fully approved until the Medicare enrollment process is complete.
Medicare enrollment through PECOS is rarely fast. For organizations without existing Medicare billing infrastructure, enrollment can take several months, including completeness reviews and CMS follow-ups.
Submitting an ACCESS application while enrollment is incomplete creates timeline risk. Participation beginning July 5 depends on enrollment status before operations start, not after.
Go/No-Go guidance
- YES, actively enrolled: Cohort 1 viable
- IN PROGRESS with recent submission: High risk for Cohort 1
- NOT STARTED: Cohort 1 unrealistic; plan for Cohort 2
Q2: Can You Submit Required Clinical Data via FHIR APIs Within 60 Days?
ACCESS requires electronic submission of clinical data using CMS specified standards. Manual data entry is not permitted. Required data includes biometric readings, laboratory values, and patient reported outcomes.
FHIR support alone does not equal readiness. Organizations must have operational APIs, mapped data elements, validated test submissions, and monitoring processes to ensure data accuracy.
Even with a modern EHR, this work typically requires multiple weeks of focused technical effort.
Go/No-Go guidance
- FHIR capable EHR with integration partner ready: Cohort 1 viable
- FHIR supported but integration not started: Possible only with immediate execution
- Legacy systems or unclear integration path: Target Cohort 2
Q3: Do You Have Health Information Exchange (HIE) Connectivity?
ACCESS participants must establish HIE connectivity within 12 months of program entry, but CMS expects you to have this infrastructure before July 5 operations begin for effective care coordination with primary care providers and referring clinicians using recognized exchange mechanisms.
Effective connectivity requires integration with regional or state HIEs, the ability to exchange standardized clinical documents, and defined coordination workflows. Market maturity varies widely, and gaps here increase operational friction during Year 1.
Go/No-Go guidance
- Already connected: Cohort 1 viable
- Connectivity in progress: Possible with immediate action
- Limited HIE availability: Participation possible but higher operational burden
Q4: Do You Have a Licensed MD or DO Serving as Medical Director With Real Authority?
Each ACCESS Participant must designate a physician Medical Director accountable for care delivery, patient safety, and outcomes oversight.
This role requires authority to approve protocols, escalate care, pause enrollment, and lead corrective actions. Without clear authority, the role becomes a compliance risk.
Go/No-Go guidance
- MD or DO identified with authority and time: Cohort 1 viable
- Candidate identified but authority not formalized: High risk unless resolved quickly
- No clear Medical Director: Delay application
Q5: Are You Prepared for Outcome Based Payment Risk?
ACCESS payments follow a quarterly payment + semi-annual reconciliation structure. CMS issues quarterly payments for validated claims during the 12-month care period (50% of total OAP), with the remaining 50% withheld for semi-annual reconciliation based on clinical outcomes and substitute service utilization. Payments are not guaranteed.
This structure creates cash flow variability, particularly in Year 1. Organizations must model downside scenarios and ensure sufficient operating capital to absorb reconciliation timing.
Go/No-Go guidance
- Financial modeling complete and risk tolerance defined: Cohort 1 viable
- Modeling in progress: Proceed only with rapid completion
- Limited financial cushion: Delay participation
Q6: Do Your Clinical Capabilities Fully Align With at Least One ACCESS Track?
Each ACCESS track requires comprehensive management of all qualifying conditions within that track. Partial participation is not permitted.
Organizations often underestimate scope requirements. Managing one condition does not satisfy track expectations if patients present with multiple qualifying diagnoses.
Go/No-Go guidance
- Full alignment with one or more tracks: Cohort 1 viable
- Minor gaps resolvable quickly: Possible with focused investment
- Significant gaps: Delay or reconsider track selection\
What to Do Next
With the April 1 deadline approaching, organizations must immediately assess technology gaps, designate accountable leadership, and initiate the right partnerships. Early cohorts gain six to twelve months of revenue timing and operational learning advantages.
Atlas by Innovaccer provides the population health infrastructure, FHIR compliant interoperability, and outcomes reporting required for ACCESS participation. We help organizations assess readiness, navigate the application process, and build compliant care workflows that perform from day 1.
Schedule a call with our experts to determine whether Cohort 1 is realistic and which track would be more beneficial for your organization and what infrastructure gaps must be closed before applying.
This is Part 1 of our three-part ACCESS Model series. In Part 2, we'll break down payment mechanics, reconciliation adjustments, and financial modeling. Part 3 will cover operational implementation, care coordination workflows, and performance optimization strategies.


.png)






.avif)









.svg)
.svg)

.svg)

