Seeing the Unseen: How Real-Time Data and Analytics are Revolutionizing Medicaid Oversight

.png)
Medicaid stands as the backbone of the American health safety net, serving over 72 million people across the country (1). But as the program has expanded, so have the demands placed on the state agencies tasked with managing it. Between post-pandemic enrollment surges, shifting federal mandates, and heightened public scrutiny, the job of a State Medicaid Agency has never been more complex or more critical.
And now, with the passage of the 2025 One Big Beautiful Bill Act (OBBBA, or H.R. 1), the stakes have been raised even further. The law introduces sweeping changes to Medicaid oversight, financial transparency, and fraud prevention placing new expectations on states to deliver measurable outcomes, with greater speed and accountability than ever before.
Fortunately, the tide is turning. A new era of real-time Medicaid analytics is redefining what's possible for state agencies, offering the kind of instant clarity and oversight that used to be months away. Here’s how this shift is not just transforming operations, but also telling a new story of smarter governance and healthier communities.
From Hindsight to Foresight: Real-Time Oversight in Action
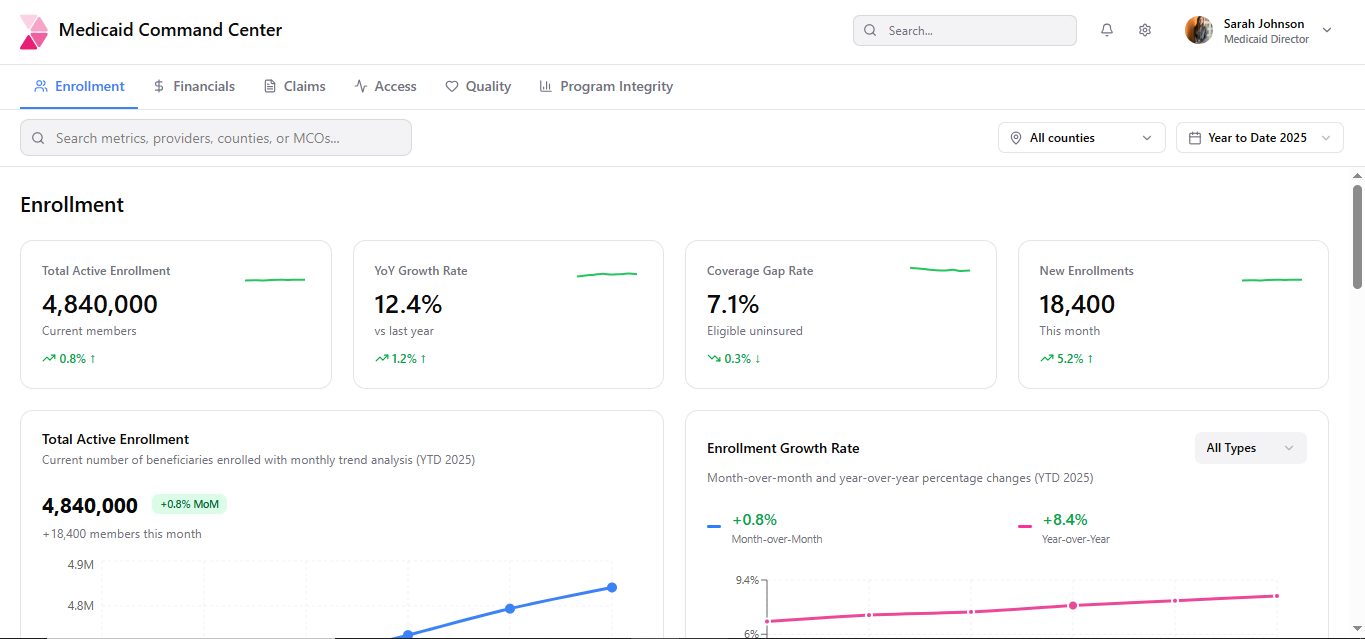
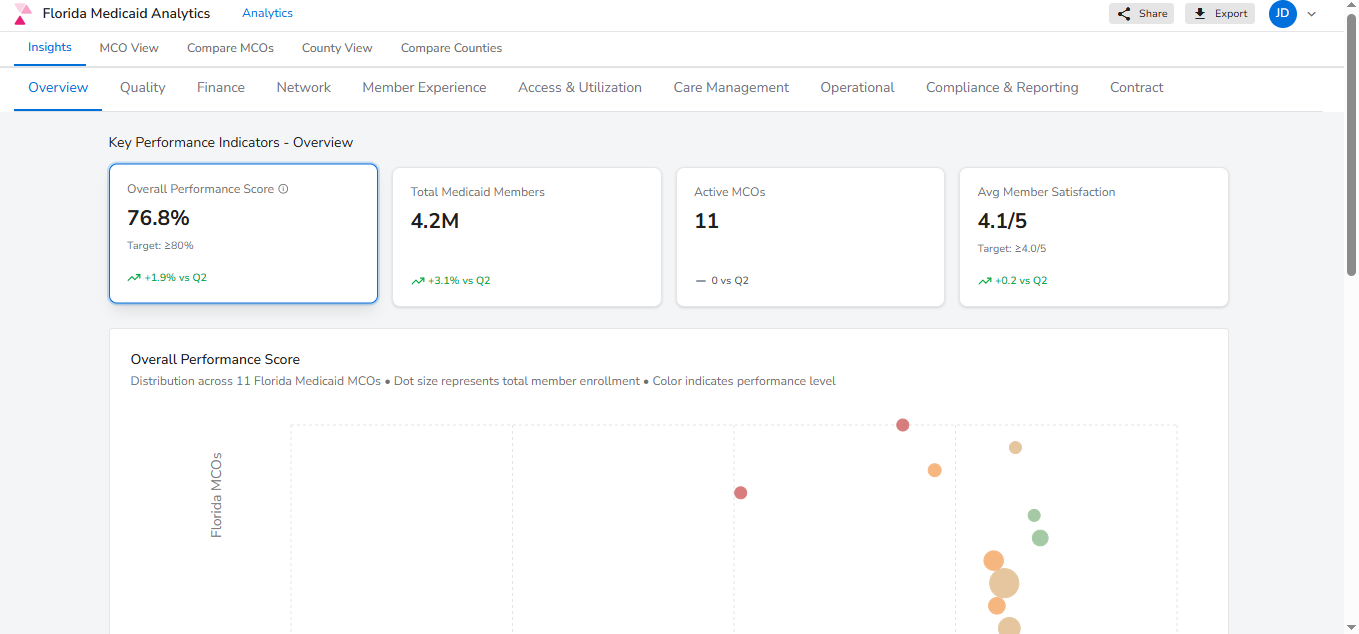
There was a time when Medicaid officials had to wait months for performance data and by then, any issue was yesterday’s problem. But platforms like Innovaccer’s Modern Medicaid Dashboards, including the Command Center and MCO Performance, have rewritten the playbook.
Command Center
MCO Performance
Now, decision-makers can see what’s happening in their programs as it happens from sudden dips in renewal rates to churn patterns threatening continuity of care. Budget variances, per-member costs, and federal matching rates are no longer mysteries; they’re live metrics that allow fiscal issues to be addressed before they spiral.
This real-time awareness doesn’t just empower internal teams, it transforms how states engage with legislators. No more waiting for quarterly summaries. With evidence-based insights, agencies can back policy proposals with real data, strengthening transparency and credibility.
Use case: During the pandemic unwinding period, states using real-time dashboards identified and addressed eligibility barriers swiftly, preventing widespread coverage losses and ensuring smoother transitions.
Today, with H.R. 1 increasing federal expectations for timely eligibility processing and financial transparency, states are under pressure to monitor enrollment patterns and program costs with greater speed and precision than ever before.
Bridging Priorities: Staying Ahead of State and Federal Mandates
Compliance today is a moving target. From T-MSIS to MCPAR, states must keep pace with evolving federal regulations while advancing their own program goals around access, efficiency, and service delivery. Doing both at scale with already overburdened resources and fragmented, siloed systems isn’t feasible anymore in this new Medicaid era.
This is where centralized data and analytics platforms prove essential. By unifying eligibility, claims, financial, provider, clinical, and health related social needs data into a single, audit-ready system, agencies can respond to federal requirements quickly and confidently while still driving localized improvements that reflect their populations' needs. Real-time dashboards surface anomalies early, enabling proactive engagement before issues become audit liabilities. Automated validations also reduce reporting lag and increase accuracy, easing the burden of quarterly reporting and annual submissions.
H.R. 1 takes this compliance challenge a step further by requiring that State Directed Payments (SDPs) include standardized reporting formats, clearly defined performance metrics, and public-facing transparency around how funds are distributed and what outcomes they drive.
Example: A state can now track and display how much of its SDP funding goes to rural hospitals, what services were delivered, and whether access or utilization improved all through a centralized dashboard.
With this kind of integrated infrastructure, states can avoid compliance gaps while also demonstrating clear fiscal responsibility to CMS, lawmakers, and the public.
Raising the Bar: MCO Accountability through a New Lens
With over 75% of Medicaid beneficiaries now enrolled in managed care, tracking MCO performance is mission-critical (2). And not just for internal optimization: lawmakers, CMS, and the public all demand visibility.
Through performance dashboards, states can benchmark MCOs side by side on HEDIS scores, member satisfaction, grievance trends, and retention. Visual indicators highlight areas of concern or success, guiding technical assistance where it's most needed.
But these dashboards don’t just compare, they narrate. Trends and heat maps bring context to the data: Why did denials spike in a certain region? What caused a surge in member satisfaction last quarter? These clues turn oversight into a dynamic feedback loop.
States can even go public with dashboards and scorecards, cultivating transparency and competition that drive MCOs to raise their game.
H.R. 1 reinforces this transparency by requiring states to publish public dashboards on MCO access, service delivery, and performance empowering oversight bodies and constituents to track how Medicaid is working in their region.
From Data to Impact: Powering Population Health with Cohort Intelligence
At its heart, Medicaid is about people. And now, advanced population health analytics help states serve those people more effectively than ever.
Using cohort tools, agencies can stratify members by health conditions, care needs, or social factors. Want to identify pregnant women in areas with high maternal risks? Need to focus on dual-eligible members likely to face hospitalization? These questions used to take months to answer, today, they’re just a few clicks away.
Risk stratification modules allow for targeted interventions, whether it's outreach to children missing well visits or deeper support for behavioral health needs. That’s not just efficient; it’s equitable.
Practical impact: One state used cohort analytics to redesign maternal health outreach, focusing on high-risk zip codes and reduced adverse outcomes by double digits in just two years.
The Future Is Watching: Real-Time Is the New Readiness
The reality is simple: Medicaid’s complexity demands better tools. Today’s public health leaders are meeting that challenge with real-time analytics that enable them to:
- Monitor financial and enrollment trends daily
- Benchmark MCOs on outcomes, compliance, and quality
- Streamline CMS reporting and reduce audit exposure
- Identify vulnerable populations and proactively intervene
- Detect and act on fraud, waste, and abuse signals early
- Track State Directed Payments with full transparency and auditability
As policy ushers in a new era of operational and fiscal accountability,real-time analytics is no longer a modernization project, it’s a strategic imperative. States that embrace AI-driven, real-time integrated data platforms today aren’t just meeting expectations, they are setting the pace for the future of Medicaid oversight.


.png)






.avif)









.svg)
.svg)

.svg)

