7 Challenges in Referral Management & How AI Can Solve Them

.png)
Referral management can effortlessly simplify a patient's healthcare experience by directing complicated cases to specialty care. The size of the global referral management market is estimated to be $42.7 billion by 2033, as per Allied Market Research. Inefficiencies, delays, and communication breakdowns, however, impede the whole process, leading to clinical and financial outcomes.
The Allied Market report identifies that 70% of referrals come from primary care visits. However, the infrastructure necessary to cope with such enormous data is not good enough yet. Adequate infrastructure demands serious investment in the form of money, which poses complexity to the entire referral procedure for the patients.
The study illustrates a startling 55-65% referral leak, wherein the patients go and see other doctors rather than the one referred to by their primary care physician (PCP) or drop the entire process altogether. The implication of such lapses directly hits the health outcome for patients, losing out on the promise of coordinated care.
Artificial Intelligence (AI) has huge potential to make these referral processes more efficient with intelligent automation, predictive functions, and data analytics capabilities that were not there before in traditional systems.
Let's dive deep into the critical challenges that organizations face in referral management:
Key Challenges In Referral Management
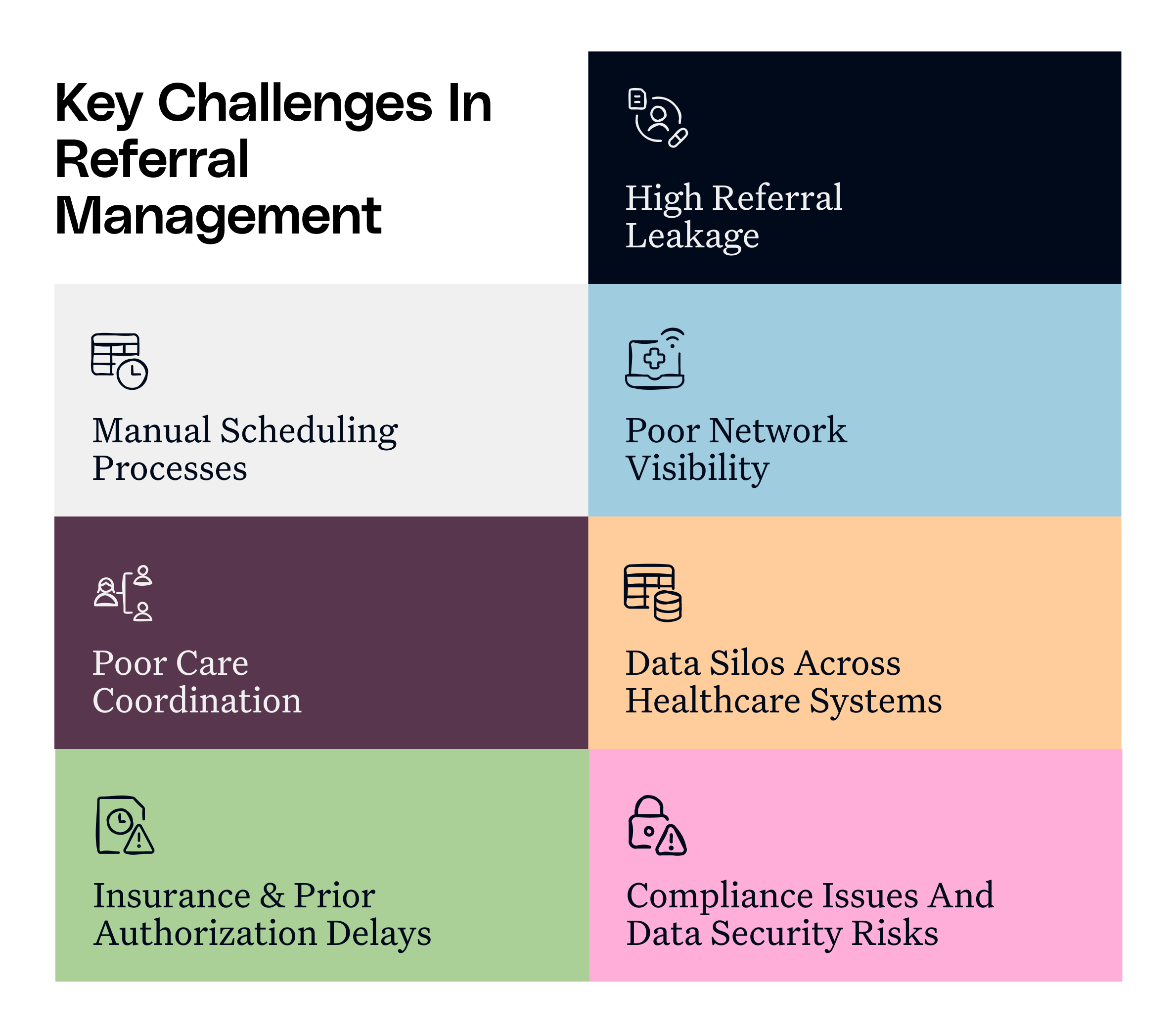
High Referral Leakage
High-level referral leakage destroys the process of referral in mid-stream, resulting in large financial loss to the organization. These incomplete referrals create delayed care, missed diagnosis, and disruption of treatment, mainly impacting complex health-challenged patients.
AI-based solutions can seamlessly avoid referral leakage with their predictive analytics capabilities. They can consider elements like access to transportation, insurance status, health literacy, and past appointment history to identify patients at risk. Organizations can then provide personalized reminders, transportation, or telehealth support to these patients. Moreover, intelligent matching algorithms can adaptively modify suggestions in real time depending on provider and resource availability to minimize scheduling delays that would otherwise have resulted in lost referrals.
Manual Scheduling Processes
Manual scheduling produces a bottleneck in referral management due to its time-consuming processes. The staff has to manually coordinate with several providers, engage in phone tag with patients, and handle intricate scheduling rules, all while coping with incessant provider availability. Paper-based scheduling is also susceptible to human errors, resulting in loss and misinterpretation of important information.
The AI solutions assist in streamlining the entire scheduling process using their smart scheduling systems. Automated scheduling assists in examining appointment patterns, provider availability, procedure types, and facility resources to reduce referral wait times. Patients are also able to get 24/7 self-scheduling capability using conversational AI interfaces and chatbots. The tools allow for easy text or voice conversation and examine clinical data to automatically inform patients with complicated cases about pre-appointment requirements.
Also read: AI vs. Traditional Scheduling: The Future of Appointments
Poor Network Visibility
Traditional referral management doesn't provide full visibility of the whole provider network, their availability, areas of expertise, and practice patterns to the primary care providers (PCP). PCPs are forced to rely on outdated directories, personal relationships, or incomplete knowledge when directing patients to specialists. It often leads to mismatched referrals increasing the possibility of referral leakages.
AI solutions bridge these gaps in information by enabling real-time visibility into provider databases. Natural Language Processing (NLP) algorithms analyze provider documentation, published research, case histories, and procedure codes to create detailed physician profiles. PCPs are then able to evaluate the provider's availability, clinical focus areas, and performance metrics to match the provider with patient needs. It provides greater transparency to patients on why a specific physician has been recommended for their care needs.
Poor Care Coordination
Ineffective care coordination among PCPs and specialists results in perilous holes in patient care, with PCPs having no idea what's happening with their patients' appointments. These failures in coordination typically lead to patients receiving redundant tests and conflicting treatments, frustrating them as they have to keep re-explaining their medical history to various providers.
AI solutions give complete visibility into the referral process via smart referral tracking and automated alerts to all stakeholders. The systems notify PCPs at each point in the appointment, providing clinical results in the form of brief summaries without manual follow-ups. Organizations can establish a virtual care team that stays in sync with patient needs via shared access to treatment plans and progress notes in a secure environment.
Data Silos Across Healthcare Systems
Critical information is trapped in isolated EHRs and independent systems that cannot effectively talk to each other. The data silos impact the referral process, particularly when critical information such as clinical information, lab results, and medication lists are not accessible to the PCPs and specialists.
The AI-based solutions consolidate siloed data through NLP and aggregation software to pull, normalize, and harmonize patients' information from dissimilar sources. The systems create comprehensive patient profiles that follow patients from beginning to end through wherever they get their treatment. The software also enables real-time interoperability among the systems, allowing for the unencumbered exchange of critical information while maintaining applicable privacy safeguards.
Insurance and Prior Authorization Delays
Manual verification of insurance and complex prior authorization forms for referral cases compel healthcare staff to spend hours browsing payer websites, submitting paperwork, and pursuing pending approvals. These administrative burdens introduce unnecessary delays or uncertainty about coverage, irritating patients and leading to referral abandonment.
AI-driven solutions do all these steps using smart automation that verifies insurance eligibility in just a few seconds. The technology automatically verifies coverage for multiple payers, pulls clinically relevant information from patient records, and automatically starts authorization requests without any human effort.
Compliance Issues and Data Security Risks
Traditional methods of sharing patient information between providers often create vulnerabilities, compromising patient-related information. Fax transmissions, unsecured emails, and paper-based handoffs can cause potential compliance issues and HIPAA violations, damaging patient trust and triggering financial penalties. These security concerns can force cumbersome safeguards that ultimately slow down referral processes and create additional administrative burdens.
AI solutions alleviate these risks by providing intelligent security frameworks that protect patient data while simultaneously enabling seamless information exchange. The systems detect and prevent inappropriate data sharing before it occurs, automatically redact sensitive information when necessary, and maintain comprehensive audit trails of all referral-related communications.
Considerations for Implementation
While referral management software is full of promise for enhancing patient care coordination, effective implementation involves close attention to this checklist of technical and human considerations:
- Organizations need to have well-defined protocols that ensure proper human oversight, especially in complicated clinical judgments that should not be entirely automated.
- They must address patient privacy issues and algorithmic bias, being ahead of the curve in the transparency of AI decision-making to engender trust from both patients and providers.
- Effective integration initiatives must be deployed to support operational needs now through long-term scalability, ensuring proper integration of fresh solutions into existing EHRs, scheduling solutions, and bill systems.
- The whole support and healthcare staff should be trained as per their jobs, emphasizing the diverse needs of diverse stakeholder groups, allowing for smoother change management practices.
By mitigating these challenges to care coordination, AI-powered referral management technologies such as Innovaccer’s solutions can empower significant improvements in both operational efficiency and patient outcomes. To know more, book a demo today!


.png)



.png)



.avif)









.svg)
.svg)

.svg)

