How Risk Adjustment Software Improve Coding Accuracy


Medicare costs continue to rise at a debatable rate. To address these rising expenses, the Centers for Medicare and Medicaid Services (CMS) has implemented various strategic value-based care initiatives. One of the initiatives is the Hierarchical Condition Category (HCC) risk adjustment model.
The HCC risk adjustment model helps to:
- Calculate cost to Medicare beneficiaries
- Enhance care delivery
- Eliminate unnecessary expenses caused by coding errors.
Given the complexities of risk adjustment, the need for accurate HCC coding becomes more critical than ever. To manage patient data and calculate risk scores on a larger scale, the need for advanced software becomes essential.
Read the blog to learn more about how risk adjustment software helps with coding accuracies.
What is Risk Adjustment and Why Does It Matter?
Risk adjustment is an evidence-based, data-driven approach. This data driven approach helps care managers to project medical expenses. To better understand patients, care teams use risk adjustment factors (RAF). These RAF scores help understand the risk profiles of their patient populations and take the required actions.
The risk profile of a patient is influenced by social determinants of health (SDOH) and the complexity of their chronic conditions. By accurately assessing patient data, care teams can predict probable costs and promote appropriate care.
The true value of risk adjustment lies in its ability to align care delivery with patient need. The process not only helps in identifying patients at high risk but also ensures that providers receive fair compensation for the quality of care they deliver.
Key Features of the Risk Adjustment Model
- Patient Demographics: Risk adjustment considers beneficiary age, gender, and other health conditions to ensure fair compensation across patient populations.
- Hierarchical Condition Categories (HCCs): The model uses hierarchical condition categories (HCCs) to modify costs based on specific health conditions.
- Cost Distribution Optimization: To allow flexibility and ensure accurate cost examination, the model optimizes cost evaluation method.
While the key features provide a framework for accurate cost prediction, their effectiveness depends on coding accuracy. And, traditionally practiced manual coding methods often fail to meet these needs.
Understanding the Limitations of Manual Coding in Risk Adjustment
Traditionally followed manual coding is prone to errors and has its own set of challenges. The process itself is time-consuming, making it difficult for healthcare organizations to operate effectively and efficiently.
The sheer volume of manual documentation and paperwork created inconsistencies in medical coding, resulting in unidentified risk scores and increased audit risk.
How can we solve these gaps?
To address the challenges posed by manual coding, healthcare organizations must adopt advanced risk adjustment software that uses different automation methods to streamline workflows and reduce errors.
How Does Risk Adjustment Software Solve Manual Coding Problems?
Manual coding is time-consuming as well as prone to mistakes. Risk adjustment software bridges this gap using advanced analytics and automated workflows. It improves coding accuracy, reduces documentation time, and improves the accuracy of the risk scores.
Accurate risk scores help care providers to analyze historical data of a patient and predict future health complications. This allows them to deliver better care and manage costs more effectively.
The AI-powered medical coding provides real-time insights directly to have better documentation and improved risk scores. Better documentation and improved risk scores help providers and payers to make informed decisions.
Let’s take an example:
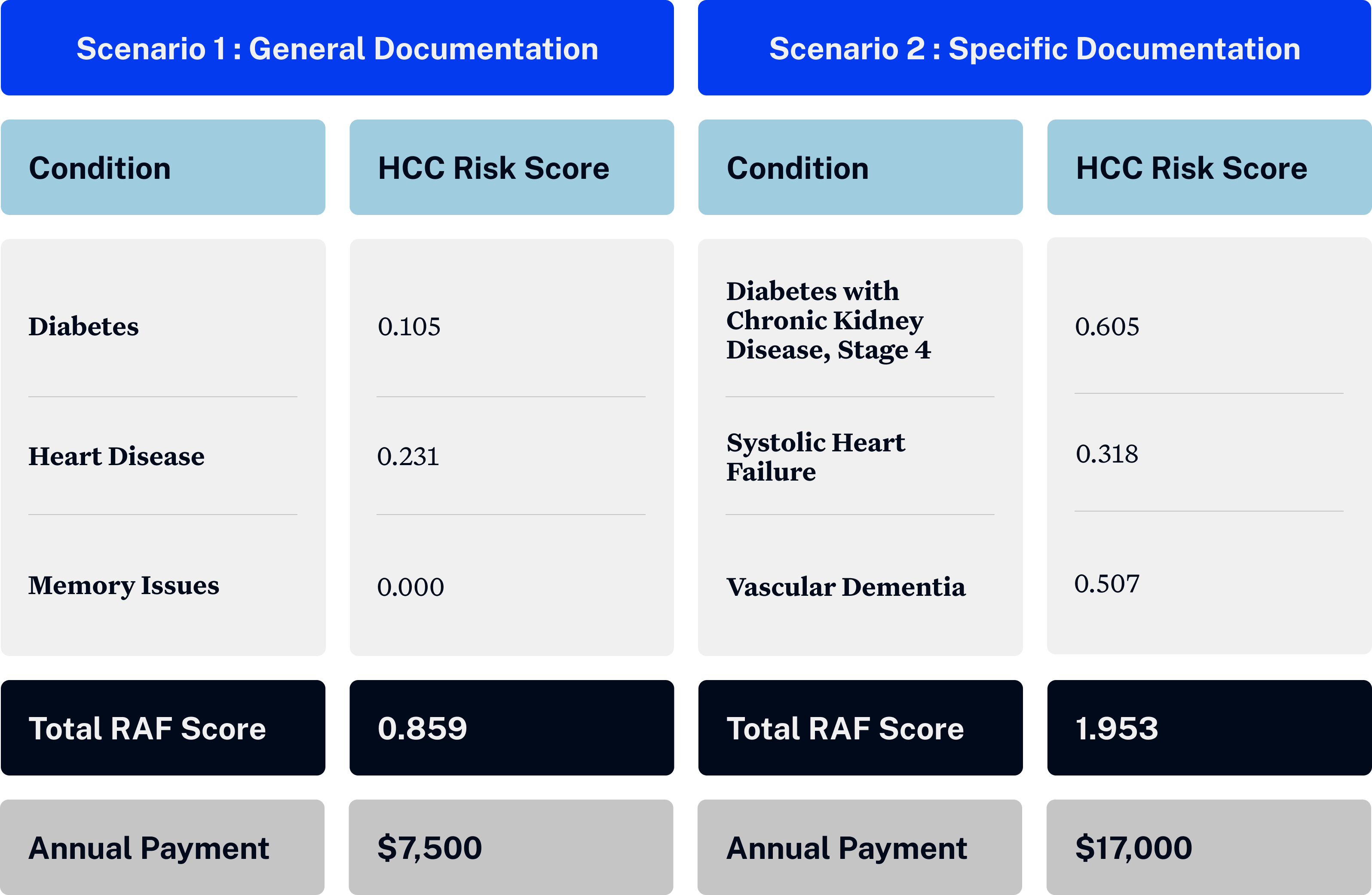
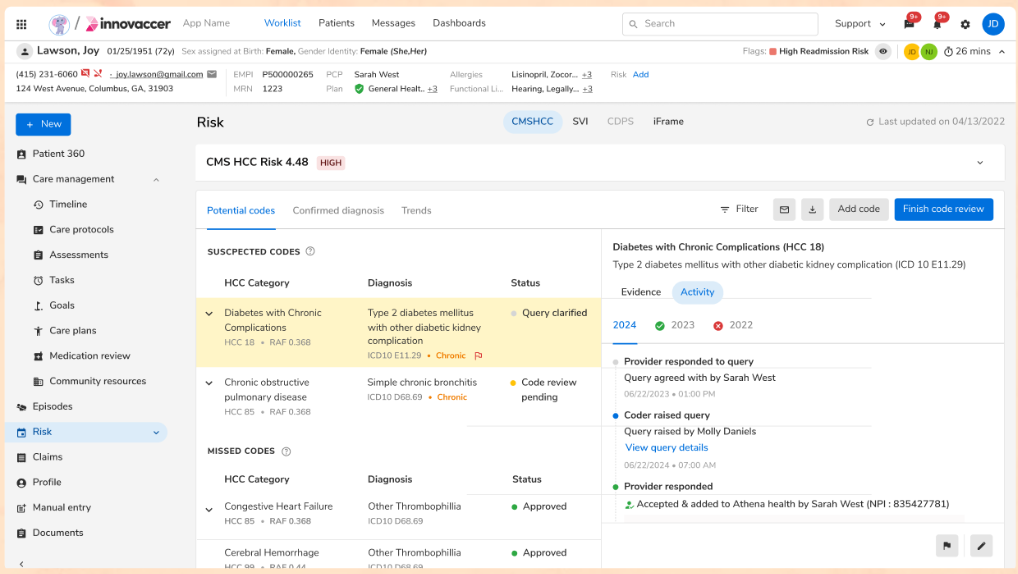
The table above shows sample data from an 82-year-old male patient with a baseline RAF score of 0.523.
The scenario demonstrates how coding accuracy in healthcare significantly impacts the patient's risk score while significantly improving financial outcomes.
- Case 1: The patient has a documented diagnosis of "diabetes," which carries an HCC risk score of 0.105.
- Case 2: The same patient has more specific documentation of "diabetes with chronic kidney disease stage 4," resulting in an HCC risk score of 0.368 for an additional 0.237 for the chronic condition.
These different documentation approaches for the same patient result in dramatically different annual member payments. This example highlights the importance of accurate and specific documentation.
Implementing an Effective Risk Adjustment Strategy
A successful risk adjustment strategy needs a clear plan. These strategies can be in the form of data integration from existing electronic health record systems or automating risk score calculations.
To overcome common challenges, it is important to follow these steps:
Step 1: Choose the right risk adjustment software. AI-powered medical coding risk adjustment software ensures accuracy and alignment while reducing audit risks.
Step 2: Choose software that can analyze both structured and unstructured data. This gives a complete picture of patient risk.
By following these steps, healthcare organizations can improve financial stability while delivering better patient outcomes.
How Can Innovaccer Help?
With Innovaccer’s Risk Adjustment Solution, clients see up to 30% improvement in coding accuracy, with a significant reduction in documentation time. The platform integrates directly with all major EHRs, automating data ingestion and streamlining information for real-time updates.
Innovaccer’s HCC coding software uses advanced natural language processing and predictive analytics to identify missed opportunities.
Key solutions that support risk adjustment include:
- InNote: Provides AI-driven clinical insights at the point of care, helping providers identify and close risk gaps in real-time.
- InCare: Supports care management teams by tracking high-risk patients and ensuring comprehensive documentation.
- 360° Gap Closure Solutions: This AI-powered platform integrates data from various sources and provides actionable insights.

.png)





.png)









.svg)
.svg)

.svg)

