Top 5 Challenges of Implementing Risk Adjustment Software


Risk adjustment software hold immense potential to drive optimal financial performance and improved patient care for both providers and payers. With the help of these solutions, organizations can ensure appropriate reimbursements, enhance care coordination, and drive better outcomes by accurately capturing the health risks of populations.
However, despite its potential, implementing risk adjustment software is challenging. Many organizations struggle with scattered data, confusing compliance requirements, and reluctant providers, hindering the adoption of these solutions. To unlock the value of risk adjustment technology, organizations must proactively address these obstacles with the right strategies and solutions.
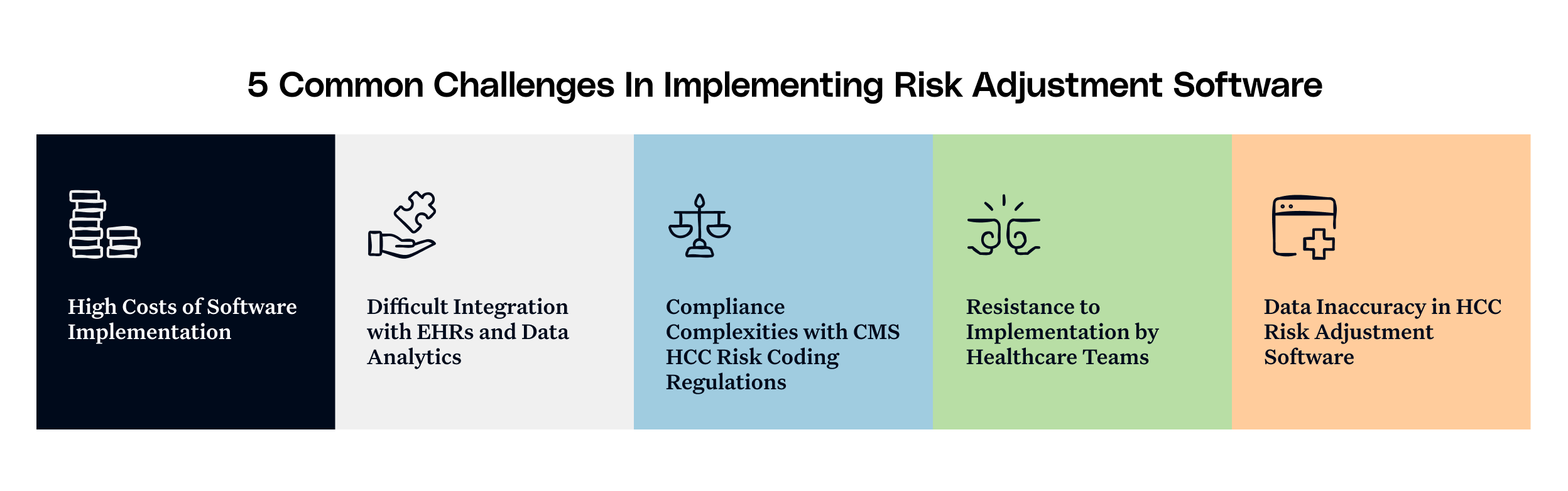
High Costs of Software Implementation
Implementing risk adjustment software can be expensive for healthcare organizations, especially smaller practices and systems in rural areas. Factors beyond software licensing impact the overall cost of the solution, such as implementation services, staff training, and potential productivity losses during the transition period. With already tight budgets, justifying this investment to stakeholders can be difficult without any understanding of the expected return on investment (ROI).
How to resolve?
These concerns can easily be tackled by understanding the ROI of these solutions and exploring flexible pricing options:
- Calculate ROI: Organizations should focus on reduced audit risks, fewer denied claims, improved quality scores, and better outcomes as key metrics to assess software implementation.
- Consider Subscription-based Models: To assess the solution’s suitability as per the organization’s requirements, they should opt for a monthly subscription-based model, avoiding any large upfront costs. The solutions can then be expanded over time, making budgeting more manageable.
- Opt for Incentive Programs and Share Resources: Organizations can easily recover costs by opting for performance-based pricing models and showcasing revenue improvements to cover costs. They can also share software costs and collectively benefit from the technology with multiple providers through a shared plan.
Difficult Integration with EHRs and Data Analytics
Electronic Health Record (EHR) structures incur huge costs for organizations, without considering a crucial element - these systems weren’t particularly designed with risk adjustment in mind. When siloed data comes into play, most of the clinical data in these EHRs becomes more unstructured. This integration challenge leaves clinical staff frustrated due to missed coding opportunities and duplicated workflows.
How to resolve?
Organizations need to consider both technical and operational factors for the successful EHR integration of the software. The solutions should be equipped with established APIs and NLP technology and have adequate experience in integrating with EHR systems. They must be capable of identifying potential Hierarchical Condition Categories (HCCs) from unstructured data through valuable coding techniques.
Additionally, they must ensure that consistent information flows between systems and the coding suggestions flow back into the EHR workflow, making it easier for providers to act on identified gaps. This approach will create a seamless flow of information between systems that maximizes coding accuracy while minimizing clinical disruption.
Compliance Complexities with CMS HCC Risk Coding Regulations
The regulatory environment surrounding risk adjustment is complex and constantly evolving, with the Centers for Medicare and Medicaid Services (CMS) frequently updating HCC models, coding guidelines, and audit protocols. Any compliance failures with the regulations can result in potential financial penalties for the software, damaging the reputation of the organization.
How to resolve?
A compliance-centered implementation strategy should focus on:
- Prioritizing Compliance Features: Software should have built-in compliance checks, coding validation, and documentation requirements for each HCC.
- Establishing Ongoing Training Programs: Organizations should conduct regular education sessions on coding updates and audit findings to keep staff updated on best practices.
- Implementing Internal Auditing Processes: The solution's analytical capabilities should be leveraged to conduct regular internal audits before submitting any claims.
- Documenting Clinical Rationale: Organizations should ensure that the software provides thorough documentation of the clinical reasoning behind each coded condition.
- Staying Updated With Regulatory Changes: Organizations should partner with vendors who proactively monitor regulatory changes and quickly update their systems accordingly.

Resistance to Implementation by Healthcare Teams
Risk adjustment aggravates the ongoing administrative overload of the healthcare staff, taking time away from patient care. Without adequate support for the solution from the entire team, even the most sophisticated solution will fail to deliver its full potential. Users will either find workarounds or will simply ignore the system's recommendations.
How to resolve?
Organizations need to address the human side of implementation with equal importance as the technical aspects. Vendors should shift the hospital’s focus towards the possible clinical benefits of the software, rather than just the financial outcomes. The physicians will be willing to trust the system when heard from other peers who can advocate for its benefits.
Adding to it, organizations need to invest in role-specific training on how the solution makes each team member's job easier or more effective. Regular communication of wins and improvements resulting from the software implementation will reinforce its value and make the staff more confident about its adoption.
Data Inaccuracy in HCC Risk Adjustment Software
Risk adjustment software are effective only when the data that they are processing are credible, high-quality, and consistent. Healthcare organizations still face data quality problems, varied documentation and terminology, and isolated information matrix. This produces inaccurate risk scores.
How to resolve?
A data quality strategy must accompany any software implementation:
- Applying Pre-submission Validation: Organizations must utilize software functionalities that verify supporting documentation before the completion of HCC codes.
- Creating Provider Documentation Templates: Vendors may develop specialty-specific templates that remind providers to document essential elements required for proper HCC coding.
- Applying Retrospective Review Capabilities: Organizations must use the software's capabilities to review potentially missed codes in encounters documented in the past.
- Establishing Data Quality Metrics: There has to be extensive monitoring and reporting of documentation completeness, coding accuracy, as well as other data quality measures.
- Creating Feedback Loops: The systems should report findings regarding data quality to providers and provide actionable recommendations for improvement.
The Road Ahead
As healthcare continues its shift toward value-based care, risk adjustment software will play an increasingly crucial role in providing financial sustainability and delivering quality care. By understanding and planning for these five common challenges, healthcare organizations can optimize risk adjustment processes that benefit patients, providers, and payers alike.
We need to remember that implementation is not a one-time event but an ongoing process of improvement. By partnering with experienced vendors and focusing on both compliance and clinical quality, organizations can transform risk adjustment from a necessary administrative task into a strategic move in today's healthcare environment. Know more about how Innovaccer’s solutions will be the right choice for your organization’s risk adjustment needs.
Unlock Better Health Plans and Cost Control
Book a customized demo to learn how we can enhance efficiency, improve risk assessment, and optimize health plans.


.png)






.avif)








.svg)
.svg)

.svg)

