Built for Providers: How AI is Making Risk Adjustment Work at the Point-of-Care

In every patient visit, providers gather crucial insights about health status, risk factors, and care needs. Yet, translating these observations into accurate risk adjustment data remains overly manual and retrospective. Meanwhile, providers find themselves caught between competing demands: delivering quality care and managing complex risk adjustment requirements.
To truly support providers, risk adjustment must evolve from being reactive to intelligent and seamlessly embedded into care delivery. And that’s where AI is beginning to make a meaningful difference.
Why are the Current Risk Adjustment Processes Falling Short?
Let’s consider a busy healthcare facility where providers are expected to rush through back-to-back appointments. In such a scenario, key details such as a previously undocumented condition that hasn’t been coded this year or unusual lab results may get overlooked, especially without real-time support.
Risk codes are left uncaptured. Coding gaps widen. A referral that could've made the patient's health better didn't happen.
This is not a one-off event. It represents the daily reality of several providers, affecting revenue and compliance. At the organizational level, the challenges are even more pronounced. Teams are expected to improve RAF accuracy and reduce compliance risk while managing outdated workflows and disconnected data systems. Thus, coding audits become reactive clean-up jobs, affecting physicians and coders alike.
This highlights why value-based care organizations must adopt a smarter approach, one that goes beyond traditional and manual processes. The need of the hour is a system that minimizes human burden, works in real-time, and helps capture risk at the point-of-care itself.
.png)
Enter: Agentic, AI-powered Risk Adjustment
Now, imagine that same busy healthcare facility, but this time equipped with an AI-powered risk adjustment software that eliminates the need for manual intervention and supports physicians at the point-of-care. As the provider opens the patient’s chart, the system has already analyzed clinical history, labs, and notes. A prompt appears for a possible missed diagnosis, suggesting a code with supporting evidence within the EHR. Thus, no switching of systems and no delays.
This is the difference our AI-based risk adjustment solution creates by offering an end-to-end agentic workflow for prospective, point-of-care, and concurrent coding. The suspect rules are LLM-based, and automated workflows enhance accuracy and efficiency with little or no human intervention.
What do we mean by "Agentic"? Most AI tools in healthcare assist: they highlight, flag, or suggest. But agentic AI does more. It acts.
Here’s how it's streamlining risk adjustment:
- Precision-driven Risk Capture:Accurate risk capture begins with visibility. The AI-powered risk adjustment solution surfaces HCC coding gaps in real-time during patient visits, directly within the EHR. With instant prompts and evidence-based suggestions, providers can act without breaking workflow. Additionally, the bidirectional EMR writeback ensures that confirmed diagnoses and documentation are recorded without any duplication or delay.
- Frictionless Documentation: Clinical documentation should support care, not slow it down. The CDI Agent and AI Copilots assist with MEAT-compliant note generation by auto-linking conditions with relevant evidence. This reduces the time spent on documentation after a visit and ensures complete documentation without overburdening the providers.
- Effortless Value-based Care Performance: Capturing risk accurately is essential to succeeding in value-based care. By analyzing structured and unstructured data across EMR, lab, HIE, and claims sources, the solution uncovers hidden diagnoses and improves RAF accuracy. Providers can rely on real-time insights to close gaps in care and ensure proper risk stratification, without added manual effort.
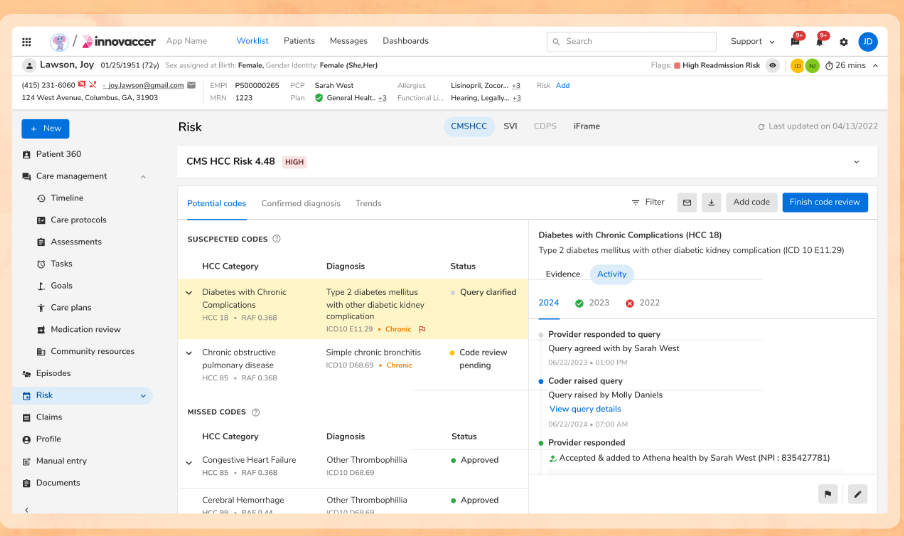
- Seamless Operational Workflows for Care Teams: The solution aids care teams as well as coders to act faster with confidence without getting stuck across data systems since it generates review-ready worklists containing suspected conditions, along with dropped conditions.
- Built-in Compliance Support: The solution not only supports accurate coding but also ensures audit readiness. It autonomously gathers and organizes clinical evidence to support each diagnosis code, creating a complete, traceable audit trail. By reducing the time and effort needed to substantiate codes, it lightens the load on physicians, coders, and care teams while strengthening compliance across the board.
Why Agentised Risk Adjustment Sets a New Standard
Agentized risk adjustment is redefining what’s possible at the point-of-care in the following ways:
.png)
This smarter risk adjustment elevates provider performance and helps organizations advance their value-based care goals.
The Next Leap in Risk Adjustment
Risk adjustment isn’t just evolving, it’s being redefined. What seemed so futuristic yesterday has become possible today with agentic AI as it reshapes the way risk is captured by providers, interacts with data, and delivers care.
By moving risk adjustment to the point-of-care as well as automating what once took hours, healthcare organizations do not just catch up; rather, they can advance, equipped to navigate the demands of value-based care.
Ready to see it in action? Make risk adjustment work for your care teams, not against them. Schedule a demo today

.png)





.png)









.svg)
.svg)

.svg)

