From Reactive Penalties to Predictive Prevention: The New Readmission Management Strategy

For 15 years, you have operated under a familiar HRRP playbook: react to penalties after they land, tweak discharge processes, and repeat. The strategy has exhausted itself.
Despite your best efforts and those of your peers, 78.6% of hospitals face readmission penalties annually. Heart failure readmissions climbed from 17.4% to 19.9% between 2016 and 2020. With operating margins compressed to 1.1 to 1.5%, you cannot absorb another $2.1M in penalty exposure while readmission costs of $17-$26 billion drain from the healthcare system.
The penalty paradigm rewards compliance reporting. It punishes your organization for patterns detected too late to change. It fragments accountability across inpatient teams, care managers, and primary care partners who never see a unified view of patient risk.
Most critically, when hospital readmissions occur at different facilities, the original hospital is left unaware until claims data arrives weeks later, long after intervention could have prevented the event.
Your old strategy is exhausted. A new one is emerging, and the window to shift is narrower than most leaders realize.
The Regulatory Crucible is Here
CMS is rewriting the structure of readmission evaluation. The performance measurement window for FY 2027 penalties spans July 2025 through June 2026. Data submission concludes in summer 2026, and penalty amounts are announced in the fall. That gives you roughly 6 to 9 months from now to demonstrate measurable improvement before performance data is locked and financial impact becomes irreversible.
Three changes activate simultaneously: Medicare Advantage populations enter HRRP calculations for the first time, COVID exclusions disappear, and the performance window compresses from three years to two.
The question becomes unavoidable. Can you continue absorbing penalties within a 1.5% margin environment, or do you build the capability to prevent them?
Fragmented Intelligence: The Bottleneck Costing You Millions
Your teams are flying blind.
At discharge, care coordinators make mission-critical decisions with partial visibility. They confirm medications and appointments, but the data that predicts readmission risk sits fragmented across systems.
Prior ED visits indicating deterioration.
Medication fill patterns revealing adherence issues.
Missed appointments signaling engagement barriers.
Social determinants correlating directly with preventable readmissions.
Behavioral patterns predicting navigation difficulty.
Your organization captures all of this. It simply does not surface when it matters: at the moment of discharge planning when intervention decisions are made.
The consequences are predictable. High-risk patients receive standard discharge protocols. Care coordination resources are allocated based on capacity, not clinical or financial need. Readmissions occurring outside your system go undetected.
For a typical 300-bed system, this fragmentation drives approximately 850 preventable readmissions every year, costing $15,200 per encounter and totaling $12.9M in avoidable expense, plus unrecovered value-based incentive dollars.
The Turning Point: Why Architecture, Not Effort, Determines Outcomes
While the pressure is financial, the solution is architectural. You cannot prevent what you cannot see, and you cannot coordinate what you cannot measure. That is the forcing function behind unified readmission management.
Organizations that are successfully cutting readmissions are changing how information flows, how decisions are triggered, and how accountability is distributed across teams. They are replacing fragmented data and manual coordination with a unified ecosystem that learns continuously and acts automatically.
This is where Innovaccer's Readmissions Management solution acts as the operational backbone of predictive prevention. It unifies data, reveals risk early, and moves action into workflow without manual lift.
One Patient, One Record: Eliminating Blind Spots
To shift from reactive response to predictive prevention, you need infrastructure that makes insight usable at the point of decision. That shift begins with the foundation that every other capability depends on.
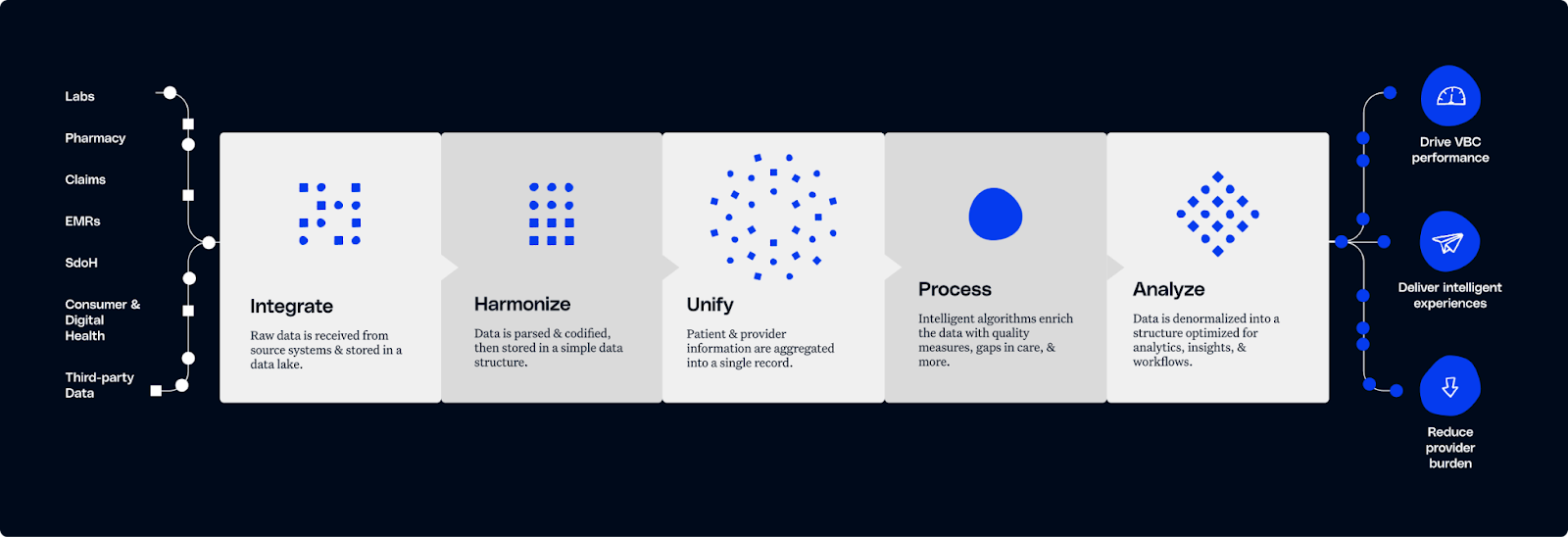
Predictive prevention is impossible when teams are working from fractured views of the same patient. Innovaccer integrates EHR, claims, ADT, pharmacy, lab, behavioral, post-acute, and SDOH data through API and FHIR interoperability.
Disconnected data arrives standardized, deduplicated, and unified into a single longitudinal record that every care team can trust.
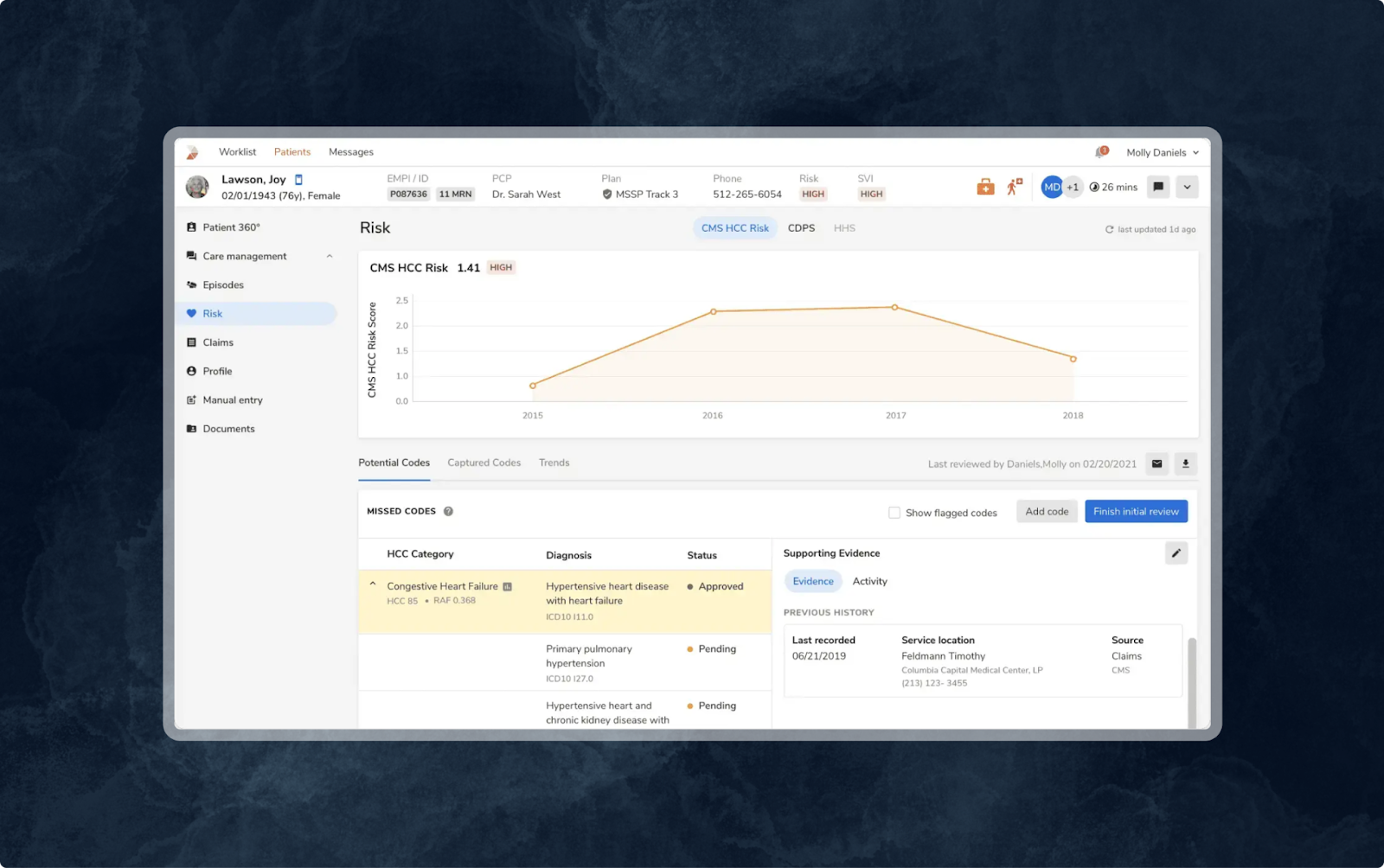
The difference is immediate. Discharge teams see and understand the full risk profile without toggling systems, reconciling information, or waiting for claims to validate what intuition suggested too late. When a patient appears in an external facility, the event surfaces instantly. Consequently, patient record blind spots disappear.
This precision also closes equity gaps. When social determinants and behavioral barriers become visible in your unified record, interventions target the populations most vulnerable to preventable readmission.
Unified intelligence turns uncertainty into accuracy and transforms intervention from a gamble into a plan.
Risk That Reveals Itself Early: Predictive Visibility at Admission
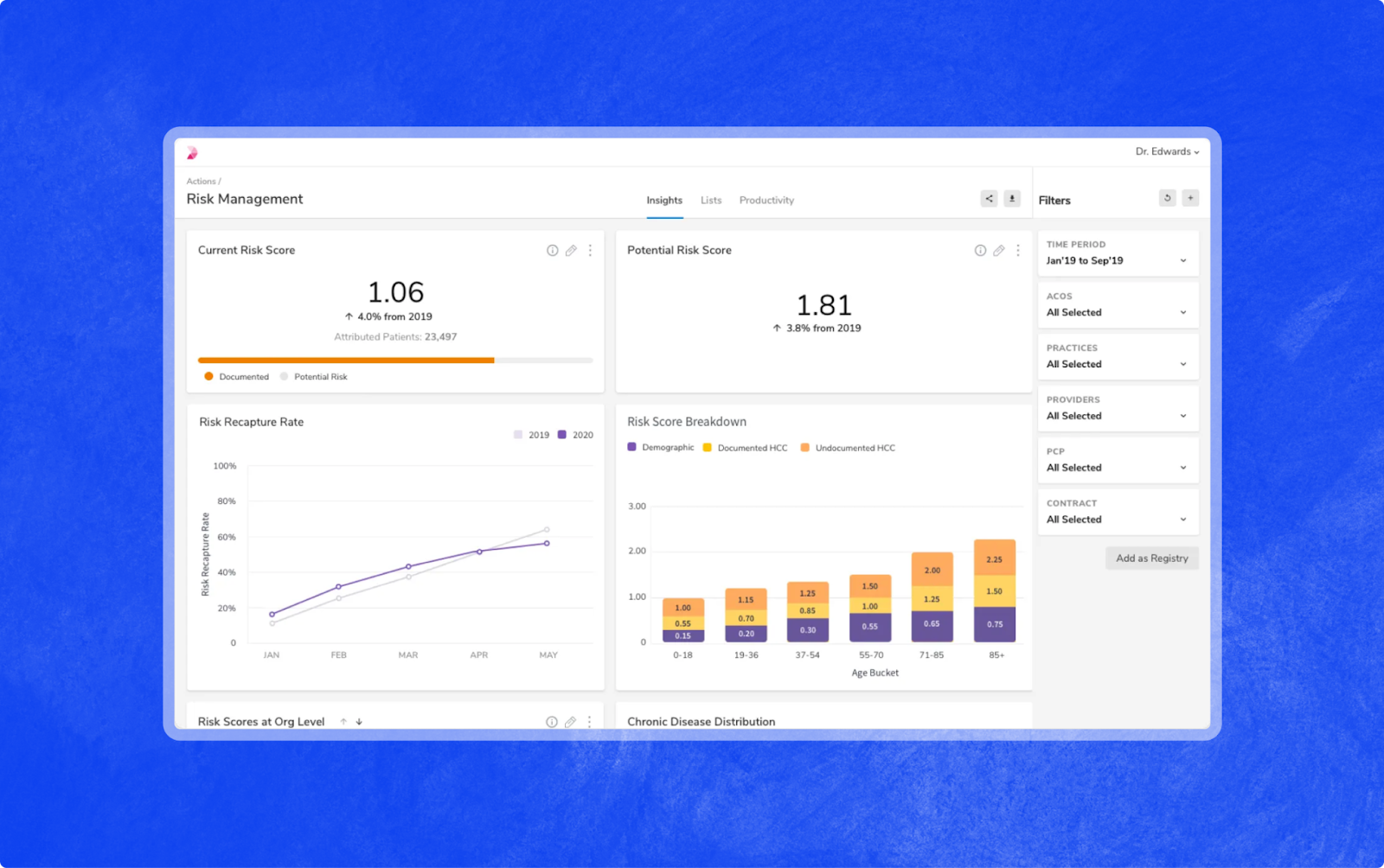
Once clinical, behavioral, social, utilization, and contractual dimensions are captured in a single record, predictive models can identify high-risk patients within hours of admission. Your teams receive a continuously updating view of who is likely to return, why they are at risk, and what levers will prevent it.
This is actuarial rigor applied directly at the point of care. High-risk patients separate clearly from standard cases. Risk drivers guide intervention choices. Leadership sees exposure in financial terms. Care teams prioritize where action matters. Precision replaces approximation. The result is resource allocation that follows risk, not capacity.
Execution at Scale: Automated Workflows That Carry the Weight
Insight has no value if it stops at observation. Innovaccer's platform moves this critical intelligence directly into the clinical workflow.
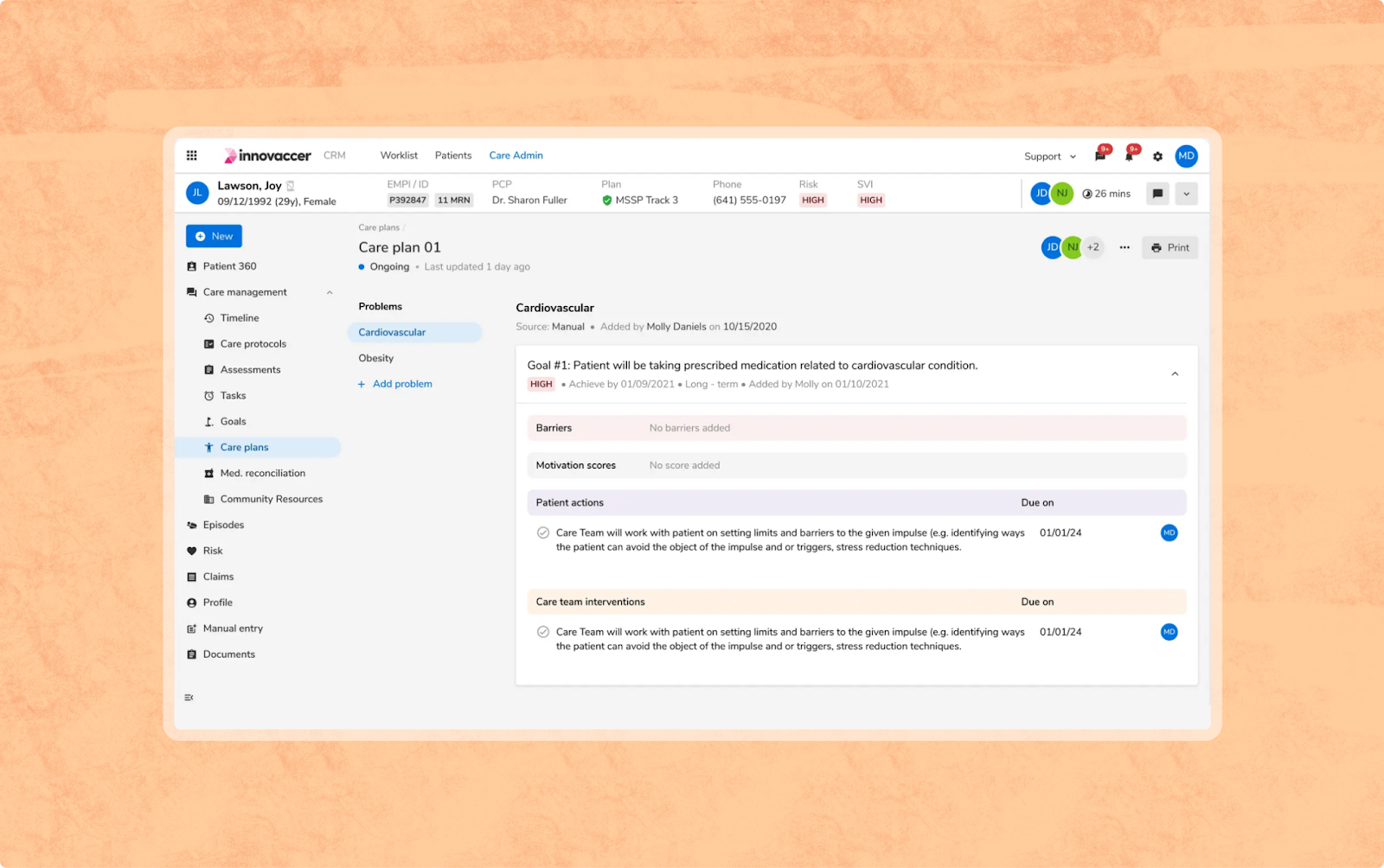
Transitional care tasks trigger automatically. Follow-up workflows route to the right navigator without manual triage. Missed appointments, non-adherence events, and early warning signals surface in real time. Alerts fire when patients re-enter emergency departments anywhere across connected networks.
Your care teams focus on what only humans can do. The system handles the rest.
Adventist HealthCare Physician Alliance Reduced 15.8% in Readmissions: The Case Study
The operational model consisting of unified data, predictive risk visibility, automated workflows is no longer theoretical. Organizations implementing this approach are demonstrating measurable impact.
Adventist HealthCare Physician Alliance, a clinically integrated network of 2,500+ clinicians managing 80,000 lives across the DC and Maryland region, provides a concrete example.
When they unified fragmented data across claims, EHR, ADT, lab, HIE, and social determinants into a single longitudinal record and automated navigator workflows, they enabled real-time risk visibility and precision intervention.
The result was clear: 15.8% reduction in readmissions, $674K in prevented inpatient costs, and $1.8M+ in MSSP savings in the first year.
Read the full case study here to see how Adventist operationalized unified readmission intelligence end-to-end.
The Gap Between Intention and Impact Closes Now
The performance measurement cycle is already underway. Data collection runs through June 2026. That gives you 6 to 9 months to demonstrate measurable improvement before results are locked and financial impact becomes irreversible.
Health systems implementing unified readmission intelligence now will have a full measurement cycle to refine processes, demonstrate results, and own the competitive standard before new HRRP metrics reshape your peer group's margins.
By the time the new metrics activate, you will have moved from reactive to predictive, turning a regulatory threat into a market advantage. The organizations that act now will define the benchmark. The rest will explain why they waited.
Book a demo with our specialists to model the financial and clinical impact of unified readmission intelligence on your specific population.


.png)



.png)



.avif)









.svg)
.svg)

.svg)

