The Ultimate Guide to HCC Coding and RAF Scoring in 2025

As healthcare moves toward value-based care, Hierarchical Condition Categories (HCC) coding and Risk Adjustment Factor (RAF) scoring have never been more important. In 2025, providers, payers, Chief Medical Officers (CMOs), and Chief Financial Officers (CFOs) are rethinking how they approach CMS-HCC Risk Adjustment. This is essential to ensure accurate reimbursement and maintain regulatory compliance as CMS continues to refine its risk adjustment strategies regularly.
This HCC Coding and RAF Score Guide 2025 covers everything you need to know, starting from how HCC coding works to proven risk adjustment best practices and how the latest HCC coding software can help your team avoid revenue leakage and compliance risks.
What Is HCC Coding?
HCC coding is a risk-adjustment model used by CMS to assess a patient's health status and predict their future healthcare costs through a hierarchical structure of diagnostic categories that assigns higher risk scores to patients with chronic illness.
The Centers for Medicare & Medicaid Services (CMS) applies its HCC model specifically to evaluate the Medicare Advantage population (patients aged 65 and older), while the Department of Health and Human Services (HHS) has developed a parallel model for the general population.
Here’s how it works:
- Diagnoses are grouped into HCCs
- Each HCC has a risk weight
- The sum of all applicable weights contributes to the patient’s RAF score
RAF scores determine the capitation payment Medicare makes to a health plan.
But importantly, precise HCC coding provides a more accurate representation of a patient's overall health, allowing organizations to understand which patients are at increased risk and how staff resources should be deployed to improve health outcomes.
Understanding RAF Scores
The Risk Adjustment Factor (RAF) is a number that denotes how clinically complex a patient is, extracted from a combination of demographic data and clinical diagnosis (HCC codes), and combinations of certain conditions. These combinations often reflect how chronic illnesses interact with each other to drive higher costs. For example, a patient with diabetes and chronic kidney disease will carry a higher RAF score than a patient with diabetes alone. This is because the interaction of these conditions leads to more complications and utilization of resources.
Medicare Advantage plans are reimbursed at rates that are impacted by RAF scores, which helps to ensure that reimbursements are appropriately related to a patient's complexity. Higher RAF scores mean more medically complex patients. This justifies higher payments to support their care needs.
Also read: Rethinking Risk Stratification in Healthcare with AI: The Future Beyond RAF Scores
Challenges in HCC Coding and RAF Scoring
Accurate HCC coding and RAF scoring can be challenging due to the following factors:
1. Incomplete or incorrect documentation
Occasionally, provider notes may be lacking in detail or have vague terms, which may limit coders' ability to capture all relevant diagnoses. This may lead to underreporting. Similarly, if the diagnoses have been placed in the wrong category, this can cause incorrect RAF score calculation and affect the organization’s revenue.
2. Risk of audits and penalties
Inaccurate coding can often show up in the case of an audit. If discrepancies are found, organizations may face fines, payment recoupments, or damage to their reputation.
3. Inefficient workflows and reliance on manual processes
Manual data entry and old workflows can create inefficiencies and result in delays in claims submissions, and impact cash flow.
4. Regular updates to CMS guidelines
CMS updates its HCC model almost every year, and changes can be extensive. It is important to constantly keep the coding team trained and informed to avoid fallouts and ensure compliance with CMS standards.
Risk Adjustment Best Practices: 5 Easy Steps to Improve RAF Scores
Healthcare providers play a crucial role in accurate risk adjustment. Here are 5 steps that you can utilize in order to improve your RAF scores:
Step 1: Review and document patient encounters
Review and document every appropriate diagnosis during each patient encounter and avoid ambiguous medical terminology. Doing this provides the opportunity to capture and report qualifying HCC conditions consistently over the course of the year.
Step 2: Leverage AI-Assisted Coding
Utilize AI-assisted coding/frameworks to review your clinical documentation in real-time and highlight the diagnoses or conditions that may have been overlooked.
Step 3: Ongoing Record Review and Validation
Continually review patient records to capture missing diagnosis codes or irrelevant codes. This will limit the prospects of claim denials.
Step 4: Close Care Gaps in Real Time
Close care gaps during patient visits instead of waiting for another appointment.
This helps to maintain accurate RAF scores and support timely care.
Step 5: Collaborate Closely with Coders
Work with coders closely to make sure every diagnosis is coded accurately.
The Rise of HCC Coding Software
Due to the drawbacks of manual risk-adjustment processes, HCC coding software has gained considerable prominence in the healthcare industry. These solutions combine automation and AI-driven insights to improve accuracy and boost real-time compliance.
Reports estimate the coding software market in the US will continue to grow at a CAGR of 9.85% by 2030.
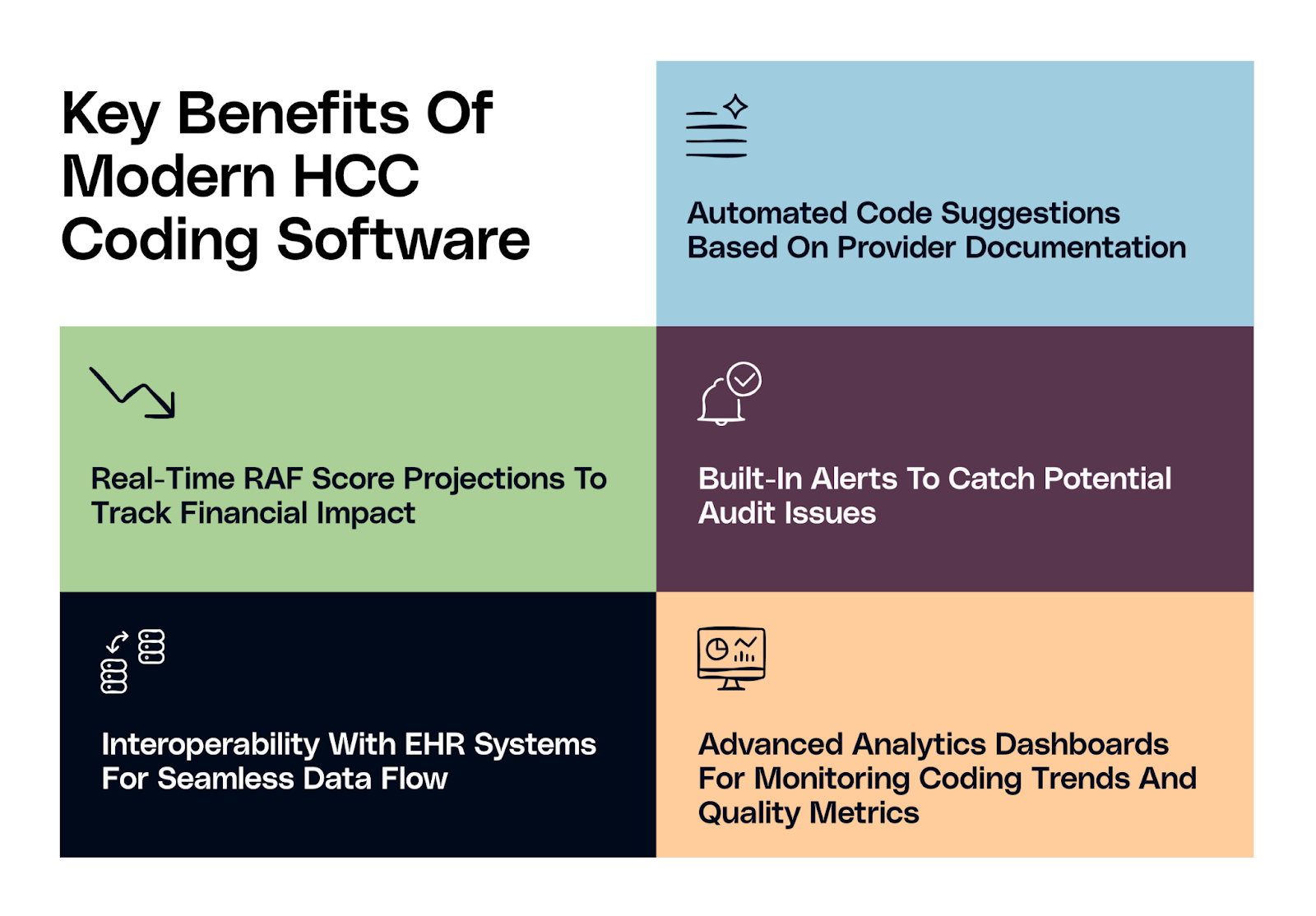
Several HCC coding software used today have AI agents working behind the scenes to identify claims and coding that may be missing from the EHR. AI agents automatically and seamlessly align documentation with the CMS-HCC guidelines, which reduces clinician burden and makes HCC coding more efficient.
Organizations that adopt AI-enabled HCC coding software will reduce administrative burden and improve RAF accuracy.
How to Choose the Right HCC Coding Solution
While choosing the right HCC coding software, organizations must look out for the following features:
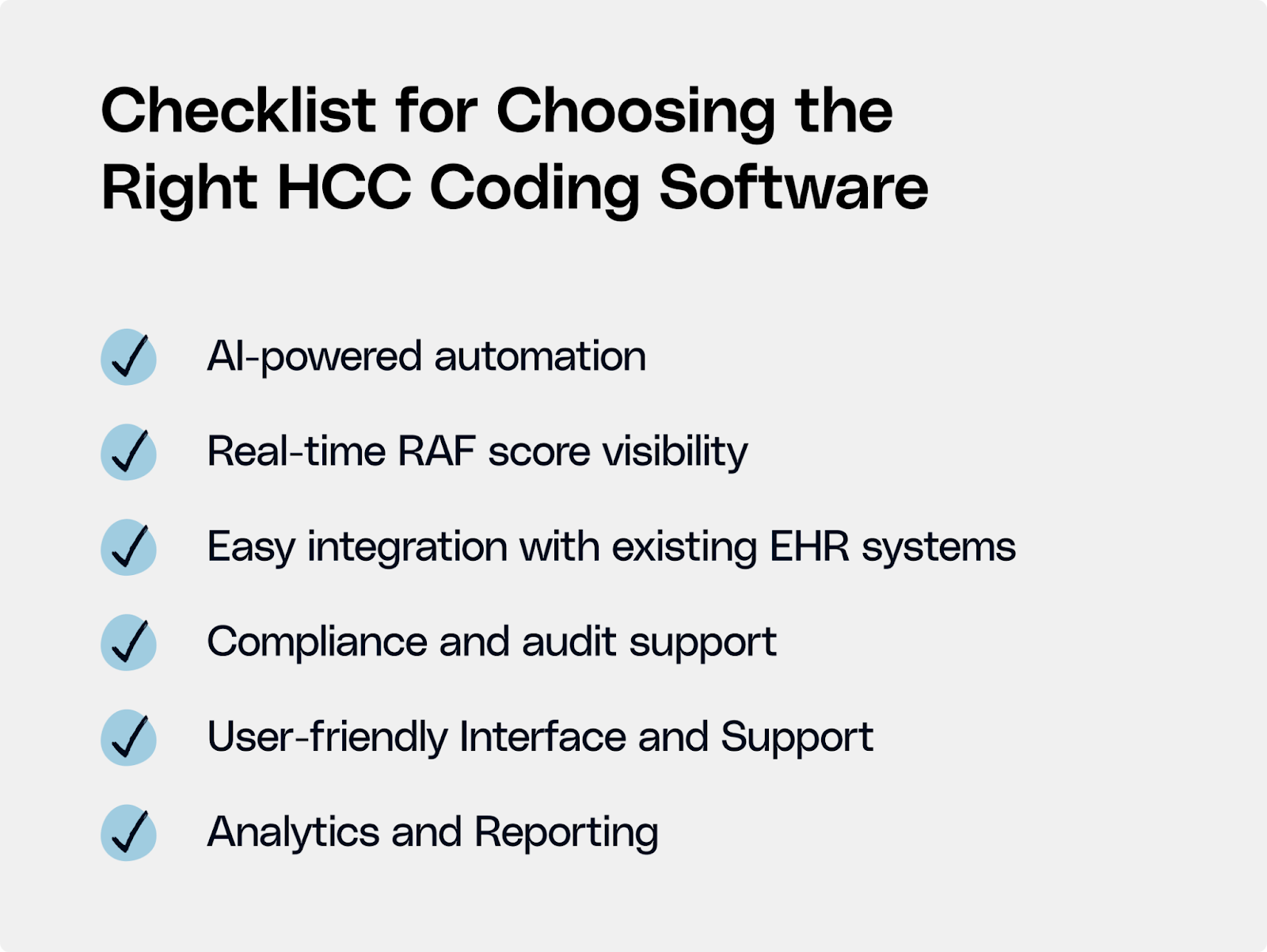
AI-powered automation
Select solutions that have advanced AI and machine learning capabilities to review clinical documentation and suggest missing codes automatically. Such a tool can improve coding accuracy and save valuable time for clinicians and coders.
Real-time RAF score visibility
Choose software that provides immediate feedback on RAF scores based on captured diagnoses. This helps care teams understand the financial impact of coding decisions and prioritize high-risk patients effectively.
Easy integration with existing EHR systems
The coding solution should integrate easily with existing systems without needing any changes to the present ones.
Compliance and audit support
The platform must flag potential audit risks early. This reduces regulatory penalties and protects the revenue cycle.
User-friendly Interface and Support
The product selected needs to have an easy-to-use interface so that clinicians and coding staff can comfortably and confidently implement the solution.
Analytics and Reporting
Advanced reporting tools provide the organization with the ability to track coding patterns, better understand opportunities for improvement, and track RAF score performance over time.
By prioritizing these criteria, healthcare providers and organizations can choose an HCC coding solution that will both simplify operations and provide better patient outcomes.
Your 2025 Roadmap to Better Risk Adjustment
Organizations need more than just basic HCC coding to stay compliant and improve patient outcomes. They must rely on AI-powered solutions to make their risk adjustment processes more efficient and maximize payments. Organizations that embrace HCC coding software will improve care and better understand their populations. Employing these technologies and best practices will be the key to surviving in the 2025 VBC ecosystem and moving beyond.

.png)





.png)









.svg)
.svg)

.svg)

