Top 5 Technologies That Help Reduce Hospital Readmissions in 2025

Lowering hospital readmissions is among the biggest challenges confronting healthcare organizations in 2025. With the transition towards value-based care models, hospitals are being required more and more to improve the outcomes of patients at a lower expense. Every avoidable readmission causes financial strain, impacts quality scores, and slows down the recovery process of patients who could be treated better.
The goal is simple: prevent hospital readmissions by sealing care gaps after discharge. But how do you accomplish that in a busy, complex health care environment? The answer lies in smart, scalable technology.
Why Technology Is Critical to Prevent Hospital Readmissions
Hospital readmissions are not random occurrences. Usually, they are caused by missed appointments, uncontrolled chronic conditions, medication mix-ups, or a lack of patient follow-up. To effectively reduce hospital readmissions, care teams need to recognize risks early on, remain engaged with patients, and act early to forestall complications.
That is where technology enters. From telehealth and remote monitoring to predictive analytics, the right care management solutions can empower care teams to make more informed decisions and offer more timely care. Employed collectively, these technologies are the foundation blocks of successful readmission management practices.
Top 5 Technologies That Help Reduce Hospital Readmissions
Hospital readmissions drive up costs and strain care teams, yet many are preventable. From predictive analytics to remote monitoring, here are five technologies helping healthcare organizations reduce readmissions effectively:
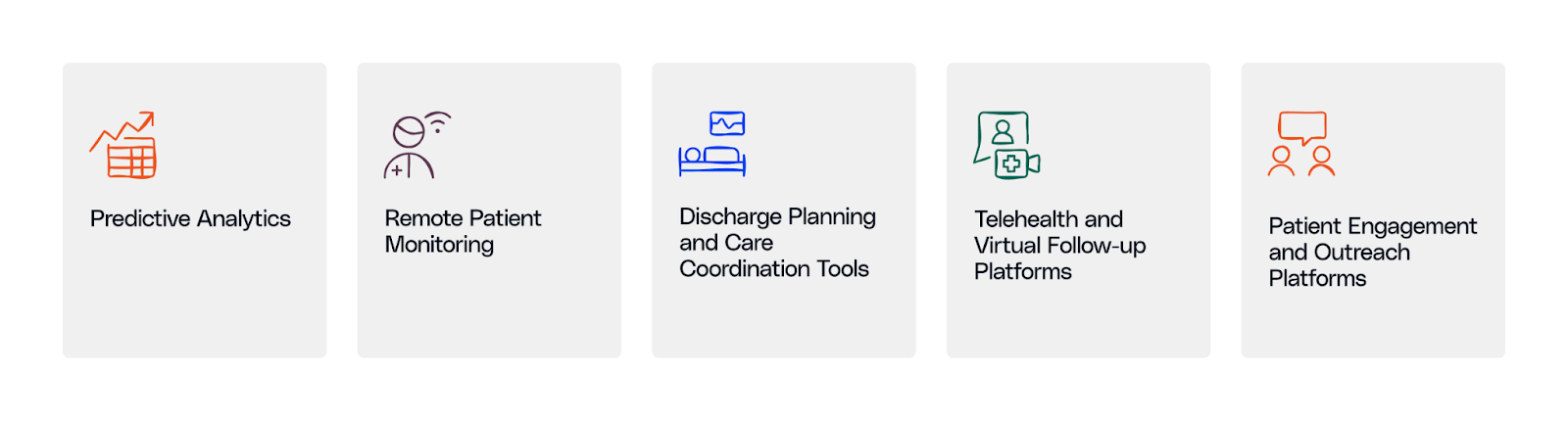
1. Predictive Analytics in Healthcare
Healthcare predictive analytics uses past and present data to determine the most probable readmitting patients. They quantify variables like previous hospitalization, comorbidities, medication adherence, and even social determinants of health (SDOH) like living or transportation.
By identifying at-risk patients early, hospitals can tailor discharge planning, offer extra support, and actively manage care transitions. Predictive intelligence allows teams to prioritize time and efforts where they matter most, which is highly essential in reducing hospital readmissions.
2. Remote Patient Monitoring (RPM)
Remote Patient Monitoring (RPM) enables care teams to remotely view a patient's status at home. Providers can monitor vital signs such as blood pressure, heart rate, glucose levels, and oxygen saturation remotely by using wearable or connected devices.
This technology is especially beneficial for patients who have complicated chronic conditions like heart failure, COPD, or diabetes - conditions that, if left untreated, typically end up causing readmissions. RPM gives early warnings and enables providers to respond promptly when something does not quite add up.
These solutions assist in:
- Early decline detection
- Keeping patients connected with care teams
- Reducing emergency visits or readmissions
3. Discharge Planning and Care Coordination Tools
A strong discharge plan can mean the difference between readmission and recovery. Yet in many hospitals, the discharge is still manual and siloed. Care coordination tools streamline the process by keeping all discharge tasks tracked, delegated, and completed. This helps prevent hospital readmissions.
These tools assist in:
- Scheduling follow-up appointments before discharge
- Giving easy-to-follow discharge instructions
- Notifying primary care physicians and specialists of recent admission
- Coordinating services like home health or transportation
Electronic discharge tools make sure everyone, including hospitalists and outpatient providers, is on the same page. That kind of consistency is key to successful readmission management.
4. Telehealth and Virtual Follow-Up Platforms
Virtual care has changed the manner in which providers check up with patients post-discharge. Telehealth platforms allow patients to see their care team via video, phone, or chat. It is easier to receive care without the aggravation of in-person visits.
The majority of readmissions occur due to failure by patients to attend follow-up appointments or adhere to care guidelines. Telehealth bridges that gap, especially for rural residents, older patients with mobility issues, or those without a transport system.
These tools assist in:
- Enabling timely follow-ups after discharge
- Identifying complications early enough to avoid deteriorating health
- Improving the ease and access to care
5. Patient Engagement and Outreach Platforms
Regardless of the quality of the discharge plan, patients need assistance along the way to stay on track. That is where patient engagement platforms come in. The platforms remind and keep patients engaged during the recovery process.
These tools assist in:
- Reminders for medication and appointment
- Provision of education via videos or articles
- Serving surveys to assess patient health
- Facilitating two-way communication with care teams
Engaged patients are more likely to follow their treatment plans, ask for help when they need it, and avoid preventable setbacks.
How to Choose the Right Technology to Reduce Hospital Readmissions
With so many predictive analysis and readmission management tools on the market, how do you choose the best one? The key is to focus on technologies that work together, are easy to use, and deliver measurable results.
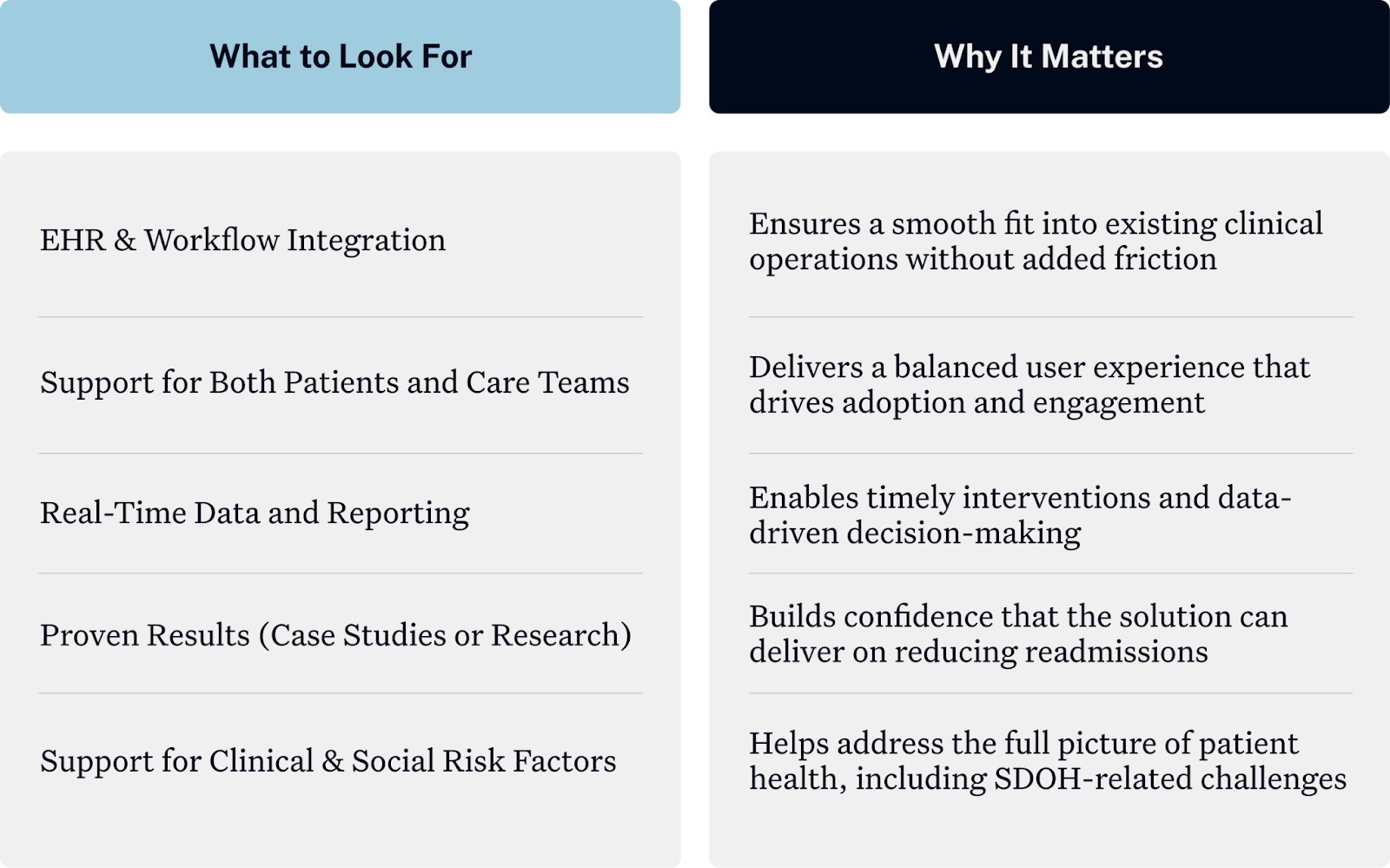
Engage clinical, IT, and operational stakeholders early in the evaluation process to drive alignment with organizational objectives and daily needs.
The Ideal Readmission Management Platform Includes All 5 Technologies
The best platforms don't provide one solution, they provide multiple technologies pulled together under one system. An ideal readmission management platform will provide:
- Predictive analytics to identify at-risk patients
- Remote patient monitoring to track recovery in the home
- Care coordination tools to accelerate discharges
- Telehealth for virtual follow-ups
- Patient engagement tools to keep patients educated and engaged
- AI copilots for population health analytics
The result? Less readmissions, better patient experiences, and better results overall.
.png)


.png)



.png)



.avif)









.svg)
.svg)

.svg)

