Readmission Management Checklist: How to Improve Readmission Rates in Less Than 60 Days

Sarah's father returned to the emergency department three times in six weeks. Same heart failure crisis. Same stabilization. Same discharge with adjusted medications that never quite worked.
He joined the 17% of Medicare patients readmitted within 30 days. According to Guidehouse Insights, each readmission costs around $15,100. For patients with chronic obstructive pulmonary disease (COPD) and acute myocardial infarction, rates climb even higher.
The Hospital Readmissions Reduction Program (HRRP) penalized over 2300 healthcare facilities in 2023, with some losing millions annually. Several government actions and CMS regulatory updates in recent years have solidified the clinical, financial, and legal need for hospitals to focus on preventing avoidable readmissions.
The problem isn't clinical care during the hospital stay. It's what happens post discharge. Primary care providers learn about hospitalizations weeks later. Patients leave confused about medication reconciliation. Skilled nursing facilities lack critical transition information.
The 60-day Goal: Is It Possible to Improve Readmission Rates This Quickly?
Yes. Central Maine Health Care reduced readmission rates by 9.8% for the MSSP population, 8.3% for the Medicare Advantage population, and 10.2% for the commercial population using predictive analytics. Another leading Iowa-based provider avoided $890K in readmissions by implementing successful transitional care management (TCM) protocols.
The secret? Target high-risk patients during three critical windows: 48 hours before hospital discharge, first 72 hours home, and the following 27 days. Electronic health records now identify these patients with 85% accuracy.
Sixty days aligns with quality improvement cycles. It's enough time to implement a 30-day readmission checklist, measure patient outcomes, and adjust strategies.
Readmission Prevention Checklist: 10 Proven Actions to Start Immediately
Most healthcare systems attack readmissions randomly. This checklist provides a systematic approach that actually reduces unplanned readmissions. Start with number one today, add another weekly.
1. Identify High-risk Patients Using Predictive Analytics
Stop guessing. Use electronic health records to flag patients with heart failure, chronic obstructive pulmonary disease, or acute myocardial infarction plus social determinants. Healthcare research shows these high-risk patient groups have 15-20% readmission rates.
2. Standardize Discharge Instructions Across All Departments
Every unit has different discharge forms. That's the problem. One template, teach-back verification, medication clarity. Prevents the errors that bring patients back.
3. Arrange Timely Follow-up Appointments Within 7 Days
Don't tell patients to "call for an appointment." Schedule it before they leave. Seven-day follow-ups cut readmissions by 12.7% as per a study published in the Journal of Critical Care.
4. Enable Remote Patient Monitoring for High-risk Populations
Give heart failure patients a Bluetooth scale. COPD patients get pulse ox monitors. When readings drift, nurses call before the crisis. Cuts readmissions in half.
5. Use Transitional Care Coordinators
One person owns each discharge. They handle everything: appointments, meds, transport, follow-ups. No shared responsibility that means no responsibility. Each coordinator prevents 4-5 readmissions monthly.
6. Create a 30-day Readmission Checklist for Clinicians
Specialty-specific. Five to seven items max. Medication reconciliation, education verification, follow-up confirmation. Non-negotiable completion.
7. Monitor Medication Adherence and Reconciliation
According to the systematic review and meta-analysis published in 2023, between 15.4% and 22.2% of drug-related hospital readmissions in older adults were deemed preventable. Conduct thorough medication reconciliation at every transition. Call patients within 72 hours post discharge. This basic intervention transforms patient safety.
8. Launch Patient Engagement Campaigns
Text beats pamphlets every time. Send medication reminders. Check symptoms. Engaged patients readmit 20% less.
9. Engage Primary Care Providers Pre- and Post-discharge
PCPs finding out about admissions weeks later? That's the problem. Alert them immediately. Send summaries in 24 hours. Cuts readmissions proactively.
10. Measure and Report Progress Weekly
Monthly reports hide failures. Track by diagnosis, unit, provider. Weekly. Patterns emerge fast. You'll see 15% better outcomes than monthly tracking.
Sample 60-Day Roadmap to Reduce Hospital Readmissions
Most readmission programs fail because they try everything at once. This 60-day roadmap sequences your interventions for maximum impact.
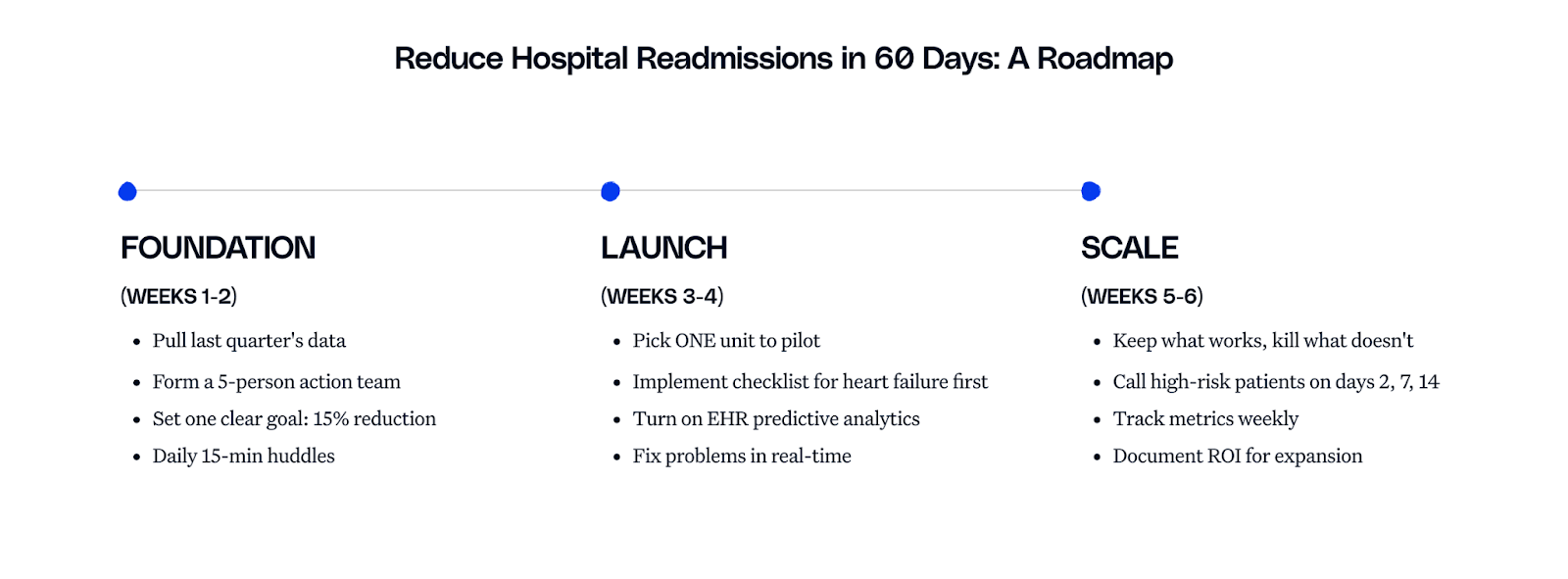
The roadmap breaks down into three phases: Foundation (weeks 1-2) where you assess and organize, Launch (weeks 3-4) where you implement core interventions on one unit, and Scale (weeks 5-6) where you expand what works and kill what doesn't.
Start small. Track weekly. Scale what works.
Tools and Technologies that Accelerate Readmission Reduction
Technology alone never reduces readmissions. But integrated with human workflows, it transforms patient care from reactive to proactive.
What makes an ideal readmission management platform? Invisibility.
💡Related read: Looking for technologies that prevent hospital readmissions by sealing care gaps after discharge?
We’ve put together a list of the top 5 technologies that help reduce hospital readmissions in 2025. Read now —>
Your care team shouldn't hunt through separate systems when a heart failure patient arrives. Risk alerts should appear in their existing workflow, flagging prior hospitalizations, medication complexity, and social factors instantly. No extra logins. No disruption.
During the hospital stay, automation matters most. Task lists for high-risk patients. Automatic compliance documentation when nurses complete discharge education. The tedious tracking of medication reconciliation and appointment scheduling? The system handles it.
Post discharge reveals the real value.
Day 2: automated check-in call
Day 7: another touchpoint
Day 14: final safety net
A COPD patient mentions breathing problems on day 7? Their coordinator gets alerted immediately, not after an emergency develops. Meanwhile, primary care providers already have discharge summaries, received within hours instead of the typical two-week delay.
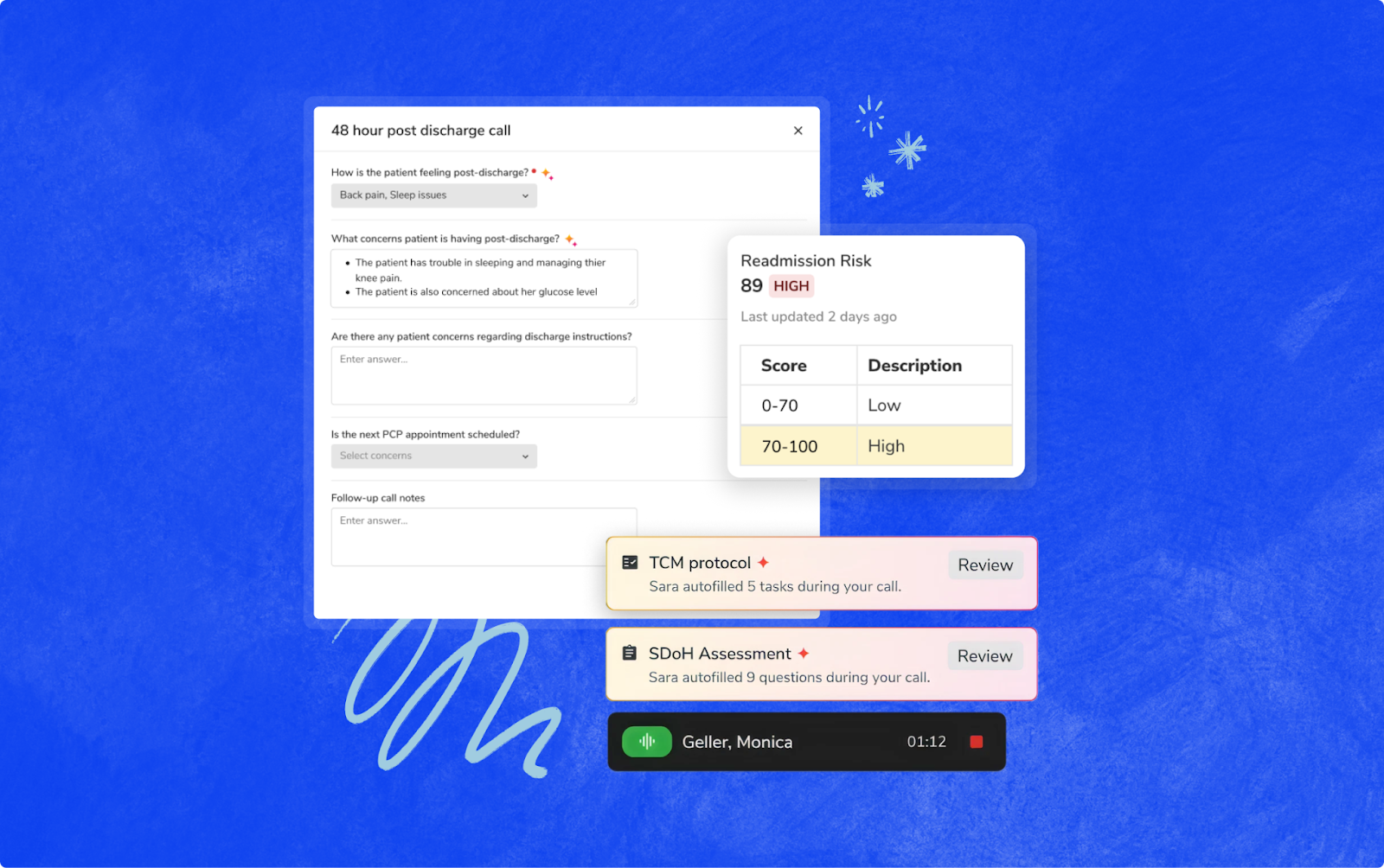
This is how Innovaccer Readmission Management works. The platform eliminates three specific failure points: missed follow-ups get caught by automated outreach, medication confusion gets prevented through reconciliation workflows, and provider communication delays disappear through instant notifications.
How to Operationalize This Checklist in Your Health System
Forget committees and lengthy planning. Success requires three committed people, one unit, and permission to try.
Start with heart failure and Chronic obstructive pulmonary disease (COPD) patients. These conditions carry substantial financial burden under payment reduction penalties.
Focus on patient safety fundamentals: medication reconciliation, patient understanding verification, and arranging timely outpatient appointments. Train staff using real patient stories in 15-minute huddles.
Make readmission prevention part of standard workflow, like taking blood pressure. That's when you've won.
Reducing Readmission Rates Starts with a Checklist, and a Commitment
Sarah's father needed comprehensive discharge planning and proper follow-up, not three emergency visits. His story represents millions of preventable readmissions straining health care systems nationwide.
This 30-day readmission checklist addresses each failure point systematically. Healthcare research and systematic reviews prove these interventions work. Organizations implementing these strategies improve patient outcomes while avoiding HRRP penalties.
Your patients deserve better than the readmission cycle. Break it now.


.png)



.png)



.avif)









.svg)
.svg)

.svg)

