Value Over Volume: How the Economics of Healthcare is Changing in the Middle East


For long, the numbers in healthcare were about activity, not impact. We were counting the number of beds occupied, the number of tests performed, and the number of procedures carried out. Under this “volume-based approach”, more activity meant more revenue, but did it mean better health outcomes? Not necessarily.
That is why the equation is now changing across the Middle East. Governments are recognizing that sustainable and effective healthcare is not about doing more, but about doing better.
For this reason, the region is betting big on value-based care, a model that ties payments to the quality and outcomes of care rather than the sheer quantity of services delivered. VBC is emerging as a critical lever for refocusing efforts on preventive healthcare rather than just treatments to improve health outcomes and savings in the long run.
The Rising Cost Challenge
A combination of aging populations and the increasing prevalence of chronic diseases is pushing costs higher in the region year after year. The number of people with diabetes in the region far exceeds the global average, with rates of 15.4% in the UAE and 18.3% in Saudi Arabia. Similarly, Obesity shows a higher average of 27.3% in the region as opposed to 12.9% globally.
The economic burden of these non-communicable diseases is immense. Saudi Arabia, for instance, estimates that public and private healthcare expenses in 2025 will touch SAR 250 billion. This is about 6% of GDP. Although this is still lower than many high-income countries, demand for healthcare is growing faster than resources. Out-of-pocket expenses still remain high in some GCC states, and many systems are fragmented with little focus on preventive care.
What does this mean for the Middle East? If the region sticks to the traditional volume-based approach, there is a high possibility that costs will continue to rise without a proportionate improvement in health outcomes. That’s where value-based care comes in.
Why Value-based Care Makes Economic Sense
Value-based care flips the incentive structure, promoting early intervention and coordinated care. These approaches reduce costly emergency visits, hospital stays, and avoidable complications. The potential impact is immense. In Saudi Arabia, VBC reforms will help save the nation around SAR 40-65 billion annually by 2035. This accounts for about 10-15% of total healthcare expenses.

How will Saudi Arabia make VBC work at scale? A critical component of this shift has been the adoption of Risk-Adjusted Capitation (RAC). Under this model, healthcare providers receive fixed per-capita payments, adjusted for patient risk profiles. This encourages investment in primary care and chronic disease management, discourages unnecessary procedures, and enables better financial planning.
For example, under RAC, instead of waiting for a patient with high blood pressure to arrive in the emergency department with complications, providers are incentivized to actively monitor their condition and ensure timely follow-ups. This approach not only improves patient health but also prevents long-term treatment expenses.

Source: Strategy& (PwC) (Transforming Healthcare Financing in Saudi Arabia, 2025)
Beyond direct cost savings, shifting to value-based care will have a much wider economic impact. By reducing unnecessary spending in healthcare, the government can redirect its funds for other national priorities, whether that’s expanding digital infrastructure or strengthening education systems. These effects align well with long-term national strategies like Saudi Arabia 2030, but the real advantage lies in building a more resilient and productive population.
How Countries in the Middle East Can Plan Better
VBC is not without implementation challenges. Many countries in the Middle East face several issues, such as a lack of digital infrastructure, fragmented care delivery models, siloed data systems, and the absence of an outcome-based payment experience. Providers may also struggle with the transition from volume to value, especially if financial and operational systems are not yet aligned.
To make value-based care work at scale, governments need to go beyond policy declarations. They must design for execution. Here are four key actions that can help countries prepare for the successful adoption of VBC:
1. Strengthen Regulatory Frameworks
Countries must first start by clearly defining how payment mechanisms like RAC will work. Everyone involved, from providers to regulators, must have clarity on who’s responsible for what. Once roles and expectations are clearly defined, it becomes much easier to ensure smoother financial operations and data flow.
2. Build Financial and Clinical Readiness
It is essential to help providers get ready for the shift by giving them the tools and training they need. This means that providers must be ready to assess patient risk accurately and design care plans that actually lead to better outcomes. Training programs on cost control and performance improvement can go a long way in helping teams adapt to this new way of delivering care.
3. Invest in Data Infrastructure
Countries should prioritize investing in the right digital tools from the beginning. The foundation for value-based care will be a robust data system where we can see a complete picture of population health. For instance, Saudi Arabia’s “National Platform for Health and Insurance Exchange Services (NPHIES)” shows how real-time processing and predictive analytics can support better decision-making. But for this to work, all stakeholders must adopt interoperable systems to make data actionable.
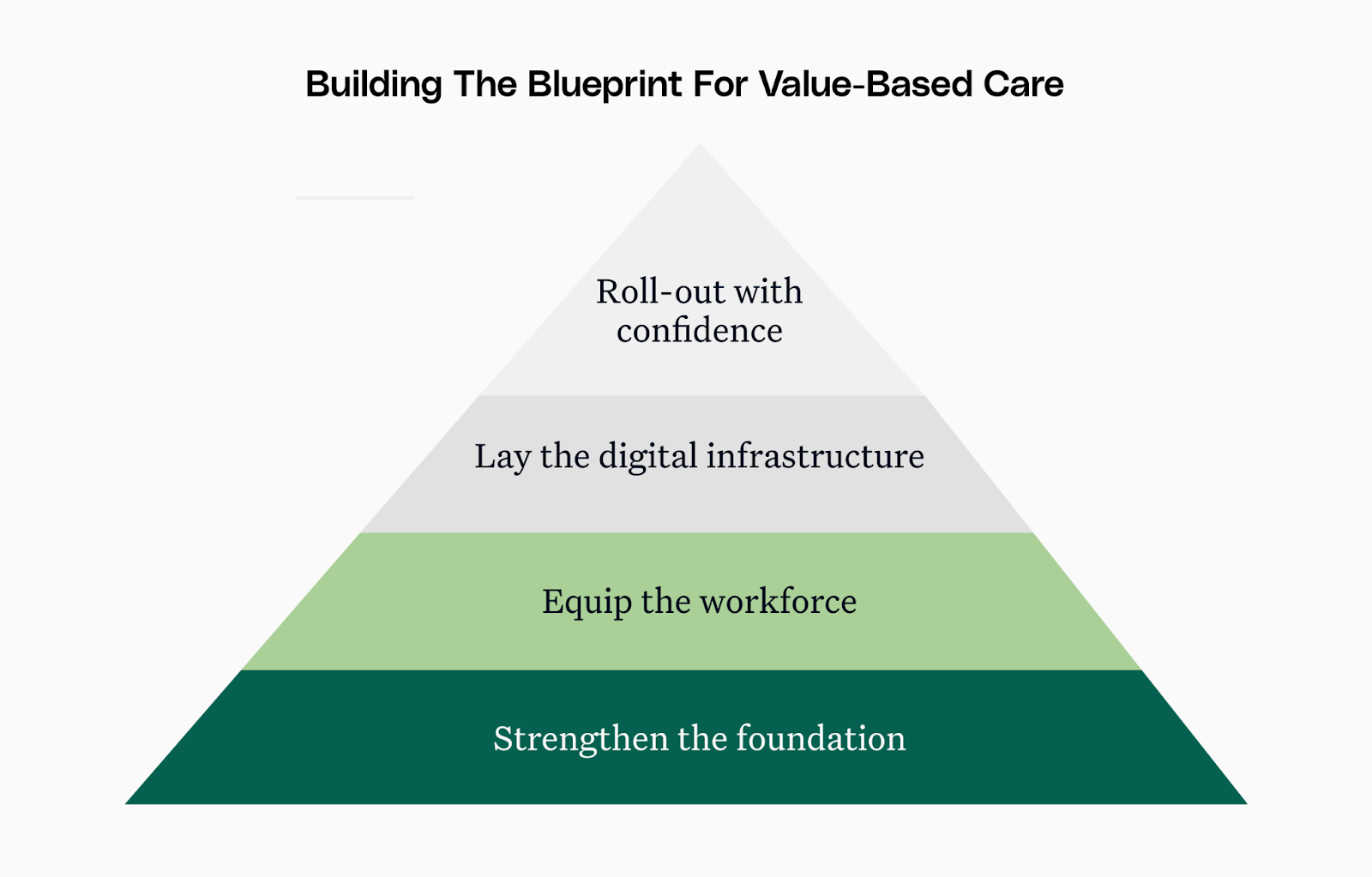
4. Implement Gradually
In many places, pilot programs are already showing what’s possible with value-based care. The key now is to build on those early efforts, gradually expanding while giving providers the support they need to fully adapt. Use the pilot process and shadow billing to better design payment models and reporting systems before rolling them out nationally. When a rollout is done in phases, it helps reduce risk and build trust across the board.
The Payoff: A Sustainable Healthcare Future
Yes, on the surface, it may look like that committing to value-based care requires a significant overhaul of existing systems. There may be a need to invest in technology or training providers. But the reward is a system that is more efficient and better equipped to handle the demands of the future without burning out the people working in it or breaking the bank for those relying on it.

.png)





.png)









.svg)
.svg)

.svg)

