EHR-Integrated Risk Adjustment: Why It’s a Must-have in 2026


Risk adjustment still happens after the fact. While physicians document care inside the EHR, coding teams often review static PDFs weeks later. This disconnect costs more than revenue. It drains time, erodes trust, and weakens competitive position.
In 2025, the math has changed. CMS expanded RADV audits from 60 to all 550 eligible Medicare Advantage contracts and grew its audit workforce from 40 to 2,000 coders (CMS, 2024). Each unsupported HCC increases recoupment risk. Each missed code is revenue competitors will capture.
The solution is not more retrospective reviews. It is embedding risk adjustment within the clinical workflow, where documentation happens and accuracy begins.
The Workflow Gap: When Coding and Care Operate Separately
Even as physician work hours decline, documentation burden remains their top frustration. U.S. physicians write notes twice as long as peers in other high-income countries. Coding teams chase documentation gaps through endless queries. Both sides lose productivity and trust.
This is not a people problem or a technology failure. It is an architecture problem. When risk adjustment in clinical workflow exists as an afterthought rather than an integrated process, everyone loses.
A 2024 OIG audit found 86% of sampled high-risk HCC conditions unsupported by documentation, triggering millions in clawbacks. Provider burnout accelerates. Audit exposure grows. Meanwhile, the market moves toward real-time, value-based contracts that assume you've already solved this problem.
What is EHR Risk Adjustment Integration?
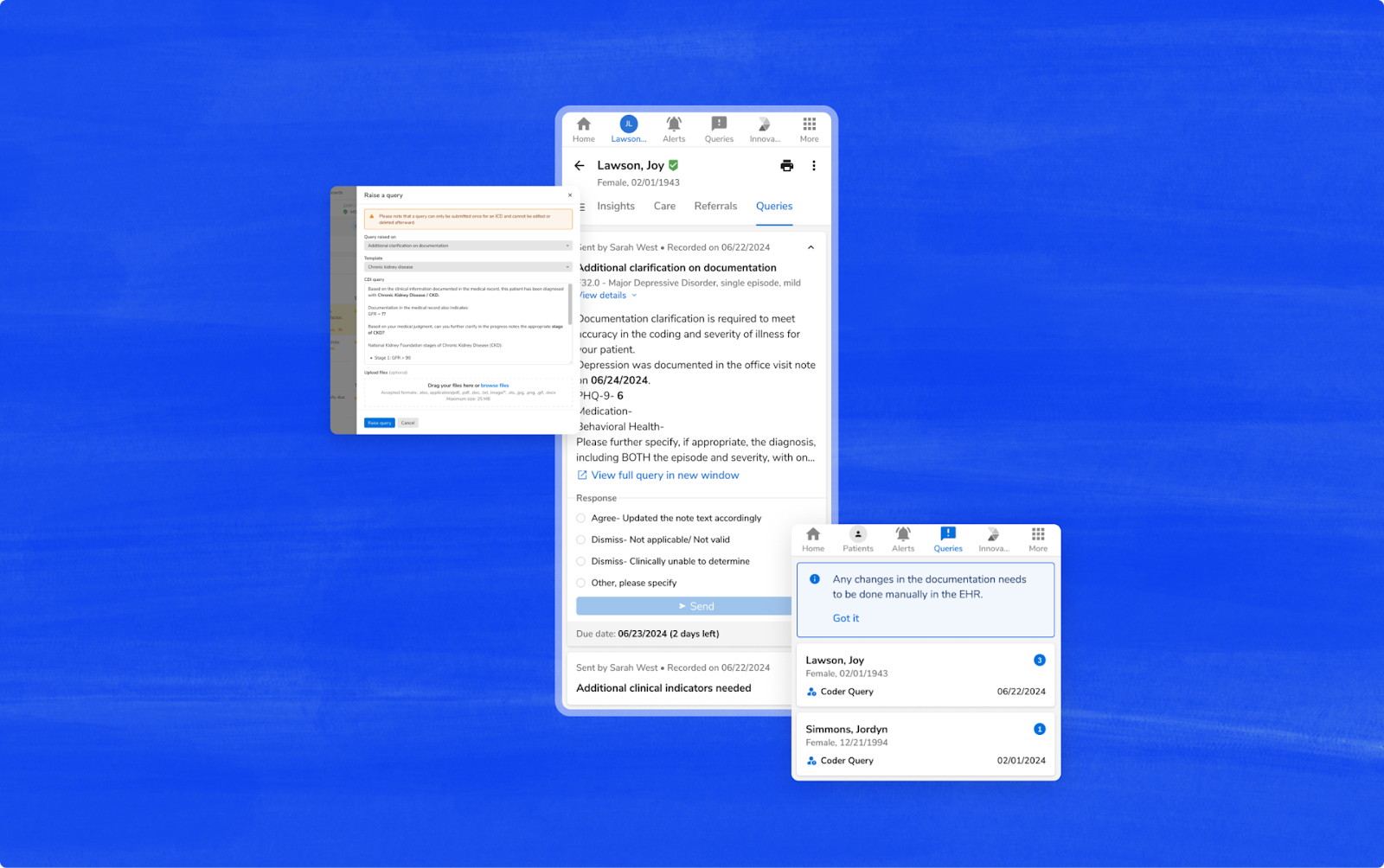
EHR-integrated Risk Adjustment embeds HCC coding capabilities directly into existing clinical documentation systems, closing the traditional gap between patient care and accurate risk capture.
It unifies documentation and coding workflows, supported by AI that reads both structured and unstructured EHR data to identify, validate, and write back codes automatically.
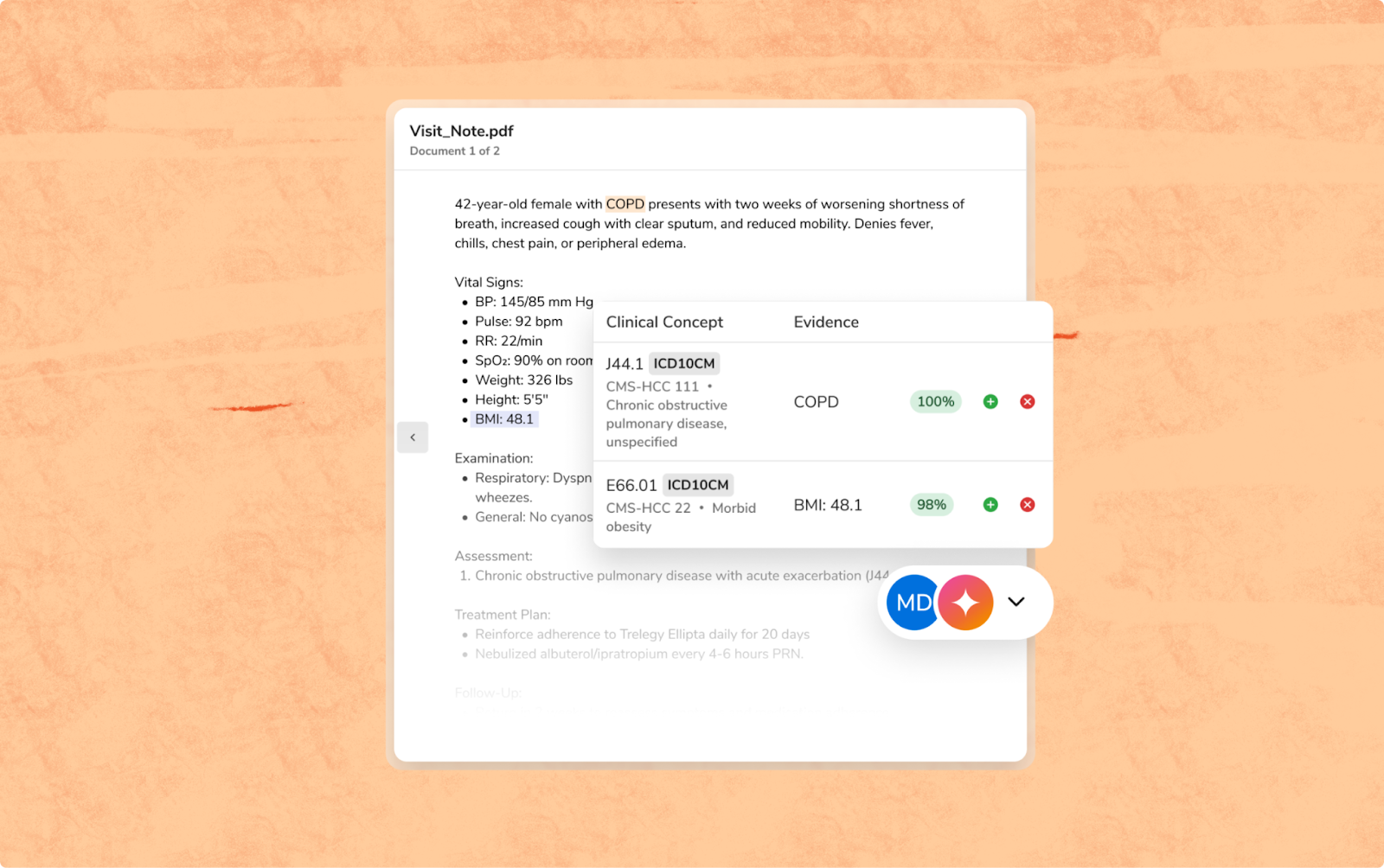
How Risk Adjustment Software Integration Works
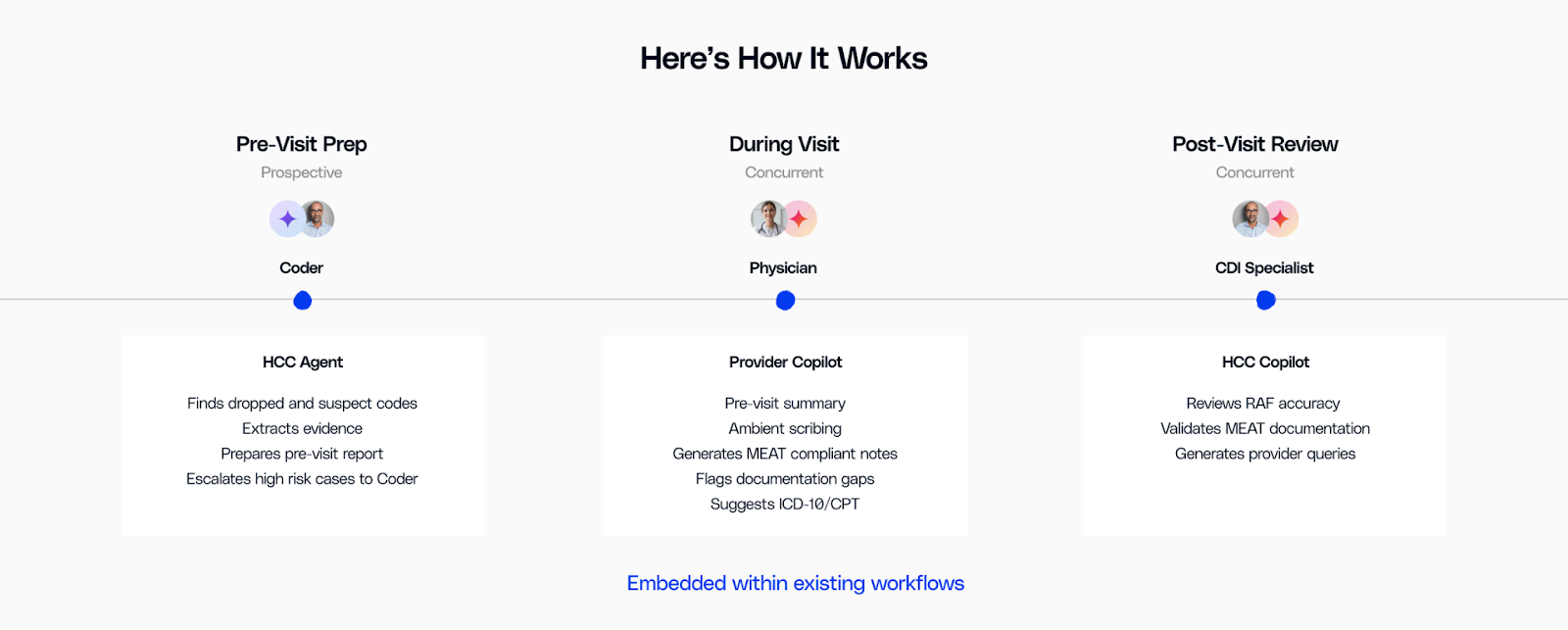
Integrated risk adjustment platforms work through three interrelated layers that turn data into real-time intelligence:
- Data Connectivity: Bidirectional APIs provide real-time data exchange between the risk adjustment platform and EHR using HL7 or FHIR protocols. Validated codes are updated to the EHR to maintain a single source of truth.
- AI Processing: Natural language processing of free-text notes extracts potential HCC opportunities. Machine learning processes diagnoses, labs, and medications, and OCR extracts data from scanned documents.
- Compliance Validation: Every suggested code is checked for MEAT criteria (Monitor, Evaluate, Assess, Treat) and CMS guideline validation for complete HIPAA compliance and audit readiness.
This architecture supports real-time evaluation. As providers attest, the system examines and brings forward applicable HCCs in seconds, with no loss of opportunity.
Real-time HCC Coding in Action
Traditional risk adjustment platforms work on a 30-60 day timeline, where coders look at past clinical encounters. Real-time HCC Coding flips that paradigm.
When the clinician enters diabetic neuropathy, the system at once identifies the associated HCC, cross-checks against CMS requirements, and requests any absent MEAT criteria.
A Texas health plan managing 36,000 lives across 12 disparate data sources implemented integrated risk adjustment within their provider network's workflows. They achieved 14% improvement in gap closure and captured 1,673 additional RAF points. Almost 99% of improvement came from opportunity capture that had been invisible in disjointed workflows. Read the full case study here.
Designing a Provider-centric Risk Adjustment Experience
A Cureus Journal of Medical Science study found that 81% of physicians report being overwhelmed by non-critical alerts on EMRs. When coding systems flood clinicians with irrelevant prompts, valuable guidance gets ignored.
A provider-centric approach filters for clinical relevance. It prioritizes high-confidence, context-specific HCCs rather than every possible code. Providers see what matters most, when it matters most.
When risk adjustment becomes assistive rather than interruptive, adoption grows naturally.
The 2025 Imperative: Why Waiting Costs More
Three forces converge to make 2025 the inflection point for EHR risk adjustment integration.
First, regulatory pressure intensifies exponentially. CMS's expansion to audit all 550 MA contracts, with extrapolation policies that multiply sample errors across entire populations, transforms documentation from important to existential. The V28 model simultaneously removes thousands of ICD codes, requiring immediate workflow adaptation.
Second, value-based contracts increasingly assume real-time risk scoring capabilities. Quarterly reconciliation no longer suffices when care management decisions require daily risk stratification. Organizations without integrated systems compete with one hand tied behind their back.
Third, the workforce reality demands efficiency. With administrative burden driving burnout, asking providers to document twice, once for care and again for coding, becomes unsustainable. Integration isn't just about revenue optimization. It's about workforce preservation.
Implementation Best Practices for Healthcare Leaders
Healthcare organizations are moving beyond asking "if" to determining "how fast" they can integrate risk adjustment into clinical workflows.
Moving from retrospective to real-time risk adjustment doesn’t require a complete overhaul. It requires a structured, collaborative roadmap:
- Assess current workflows to identify integration gaps
- Select a platform built on open, FHIR-ready architecture
- Engage providers early with training and change management
Integration succeeds when it feels invisible to those using it. The goal is to make every existing tool smarter, faster, and more connected.
From Back Office to Boardroom: Risk Adjustment as Strategy
Risk adjustment has moved from a coding function to a strategic competency. Finance teams, compliance leaders, and clinical operations now share equal stakes in accuracy.
When CMS can audit any plan at any time and extrapolate single errors into millions in recoupments, documentation quality becomes existential. When value-based contracts require daily risk stratification, integration becomes competitive infrastructure.
EHR-integrated risk adjustment is no longer a technical feature. It is the operational foundation for sustainable, compliant, and provider-led care.
Book a demo with our provider team to evaluate your integration readiness and ROI potential.


.png)






.avif)









.svg)
.svg)

.svg)

