Top 5 Chronic Care Management Software Solutions for 2025


In today’s healthcare landscape, where nearly half of the US population is dealing with multiple chronic conditions, an effective chronic care management (CCM) system is essential. Chronic care management software helps healthcare providers engage eligible patients, particularly those with multiple chronic conditions, to improve outcomes and streamline documentation. An effective solution aims to improve patient outcomes, enhance quality of life, and reduce the burden on the healthcare system’s resources.
Healthcare providers encounter numerous challenges when managing chronic conditions, such as coordinating care between providers, ensuring patient adherence to treatment plans, and handling the financial aspects. Chronic care management software is crucial in addressing these challenges. It provides a centralized platform for managing patient data and creating personalized care plans, enabling proactive interventions and ensuring continuity of care.
Moreover, by integrating predictive analytics and decision support tools, healthcare providers can gain valuable insights into patient risk profiles. These tools help identify care gaps and risk factors, enabling early intervention for patients at significant risk, such as those with at least two chronic conditions that may lead to decline or death. Care management software is especially valuable for Medicare patients and primary care providers, who are often responsible for managing complex patient populations. The role of chronic care management software is vital in enhancing patient outcomes, improving quality of life, and building a sustainable healthcare ecosystem. Adopting it also improves patient satisfaction, reduces healthcare costs, and increases practice revenue.
Introduction to Chronic Care Management
Chronic care management (CCM) is an essential strategy in modern healthcare, designed to address the ongoing needs of patients living with chronic conditions such as diabetes, heart disease, and hypertension. By providing structured chronic care management services, healthcare providers can deliver comprehensive, coordinated care that goes beyond routine office visits. CCM involves regular monitoring, medication adherence support, lifestyle coaching, and seamless communication among care teams to ensure patients receive the right care at the right time.
The use of advanced care management software is transforming how chronic care is delivered. These management software solutions streamline care coordination, enhance patient engagement, and enable healthcare providers to track and analyze patient data more effectively. As a result, care management programs are better equipped to improve patient outcomes, reduce complications, and lower healthcare costs. By leveraging technology, healthcare organizations can offer high-quality, patient-centered care that supports long-term health and well-being for individuals with chronic conditions.
Healthcare Chronic Care Management Companies: Market Overview
The United States has experienced significant growth, with the house calls segment reaching a valuation of USD 537.7 million in 2022. Projections indicate a steady upward trajectory, with an expected Compound Annual Growth Rate (CAGR) of 5.62% from 2023 to 2030.
This expansion underscores the industry’s vital role in addressing the evolving needs of a diverse patient population, particularly those living with various chronic conditions. Chronic care management companies are increasingly focused on providing scalable solutions that help healthcare organizations manage care for patients with chronic conditions more effectively. As these companies continue to innovate and expand their services, the ramifications of their advancements are evident across several critical metrics for healthcare organizations:
- Improved patient outcomes,
- Enhanced access to healthcare services,
- Reduced healthcare costs,
- Personalized, patient-centered care delivery models.
Additionally, such growth fosters opportunities for collaboration between healthcare providers, technology companies, and policymakers to further optimize care delivery and promote population health management strategies.
Key Features of Chronic Care Management Software
Effective chronic care management software is built around several key features that empower healthcare providers to deliver high-quality care to patients with chronic conditions. One of the most important capabilities is patient data aggregation, which brings together information from electronic health records (EHRs), remote patient monitoring devices, and other healthcare systems to provide a comprehensive view of each patient’s health status.
Care coordination tools are essential for facilitating communication among care team members, assigning tasks, and tracking patient progress. These features help ensure that everyone involved in a patient’s care is on the same page, reducing the risk of care gaps and improving overall care management. Patient engagement functionalities, such as educational resources, appointment reminders, and feedback mechanisms, encourage patients to take an active role in their care, which is crucial for improving medication adherence and health outcomes.
Analytics and reporting capabilities allow healthcare providers to identify trends, monitor patient outcomes, and pinpoint areas where care can be improved. Additionally, robust chronic care management solutions support remote patient monitoring, medication management, and personalized care planning, ensuring that patients receive ongoing support tailored to their unique needs. By integrating these key features, care management software enables healthcare organizations to deliver more effective chronic care and achieve better patient outcomes.
Evaluating Chronic Care Management Software
When selecting chronic care management software, healthcare organizations must consider several critical factors to ensure they choose a solution that meets their needs. Usability is paramount—the software should be intuitive and easy to navigate for both healthcare providers and patients, minimizing training time and maximizing adoption. Security and privacy are also essential, as the software must protect sensitive patient data and comply with regulatory standards.
Scalability and flexibility are important for accommodating the diverse needs of different healthcare settings, from rural health clinics to large health systems. The software should be able to grow with the organization and adapt to changing care management requirements. Strong analytics capabilities are vital for tracking patient outcomes, identifying care gaps, and supporting data-driven decision-making.
Finally, healthcare organizations should look for chronic care management solutions that are certified by reputable bodies, such as the Office of the National Coordinator for Health Information Technology (ONC). Certification ensures that the management software meets industry standards for security, privacy, and interoperability, giving healthcare providers confidence in their investment. By carefully evaluating these factors, organizations can select a chronic care management solution that supports effective care management and delivers measurable improvements in patient outcomes.
Security and Privacy Concerns
Security and privacy are top priorities in chronic care management, given the sensitive nature of patient data handled by care management software. Healthcare organizations must ensure that their chosen management software includes robust security features such as encryption, firewalls, and strict access controls to safeguard patient information from unauthorized access or data breaches.
In addition to technical safeguards, privacy features like patient consent management and data anonymization are essential for maintaining compliance with regulations such as the Health Insurance Portability and Accountability Act (HIPAA). Properly managing patient consent ensures that patient data is only accessed and shared with the appropriate parties, in accordance with legal and ethical standards. Healthcare organizations should thoroughly assess the security and privacy capabilities of any chronic care management solution to ensure that patient data remains protected and that the organization remains compliant with all relevant regulations.
Return on Investment
Investing in chronic care management software can yield a substantial return on investment (ROI) for healthcare organizations. By streamlining care management processes, these solutions help improve patient outcomes, reduce emergency room visits, and enhance patient satisfaction—all of which contribute to lower healthcare costs and increased revenue. Improved patient engagement and better chronic care management also position organizations to qualify for value-based payment incentives, such as those offered by the Centers for Medicare and Medicaid Services (CMS).
To accurately assess the ROI of a chronic care management solution, healthcare organizations should consider the total cost of ownership, including software licensing, implementation, and staff training, against the anticipated benefits. These benefits may include reduced hospitalizations, improved patient retention, and higher quality care delivery. By focusing on improved patient outcomes and operational efficiencies, healthcare organizations can make informed decisions about adopting care management software that supports both clinical and financial goals.
The 5 Best Chronic Care Management Solutions
By facilitating communication and collaboration among care teams, chronic care management software and programs can minimize fragmented care, prevent medical errors and delayed diagnoses, and assist patients in navigating the complexities of their conditions to achieve improved outcomes. These solutions support enrolled patients through streamlined patient enrollment, digital consent collection, and ongoing participation in CCM services.
Here is a list of companies that have developed technology to provide comprehensive care coordination and support for patients with chronic illnesses.
Innovaccer Chronic Care Management with a Data Platform
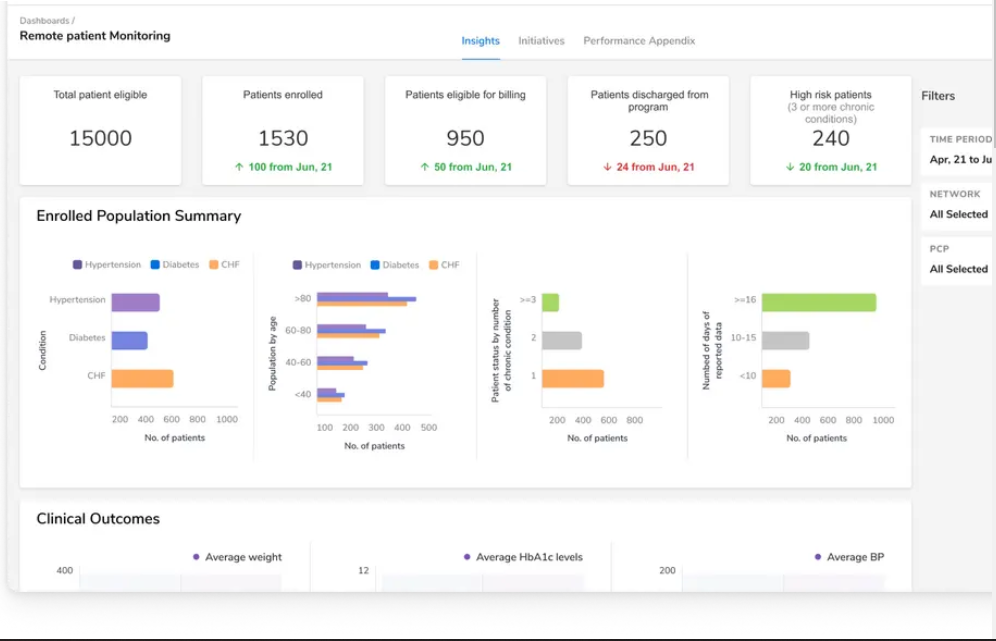
Innovaccer is a prominent player in the field of chronic care management. It has been instrumental in advancing the role of technology in care coordination and improving patient outcomes. Innovaccer has emerged as a leader in facilitating effective chronic care management with its innovative, award-winning data and analytics platform and support services. Its advanced capabilities enable real-time patient risk stratification, facilitating personalized care plans and reducing hospital readmissions. The platform also helps identify high risk patients and supports chronic care delivery for chronic care patients.
Innovaccer offers a product suite to streamline care coordination and enhance practice efficiency. Trusted by 70+ healthcare organizations, the platform aggregates and normalizes data from disparate sources, ensuring interoperability and HIPAA compliance.
With a focus on innovation and continuous improvement, Innovaccer is shaping the future of chronic care management. By harnessing comprehensive patient data, such as Electronic Health Records (EHR) and claims data, Innovaccer facilitates accurate risk stratification and personalized care planning, ultimately leading to improved outcomes and reduced costs in chronic care management.
Epic Practice Management
Epic Software is the leading EHR choice for healthcare organizations. It provides extensive support for over 40 specialties and offers customizable features to align with user needs and workflows.
Physicians benefit from a user-friendly dashboard, which grants easy access to patient charts and streamlined documentation through the NoteWriter tool. Epic’s integrated practice management software also boosts efficiency by enabling paperless billing, online payments, and automated coding, thereby reducing administrative overhead and increasing revenue. The software enables tracking of patient status, access to patient records and medical records, and supports electronic medical records and electronic health record integration.
Signallamp
Signallamp is a highly favored chronic care management company renowned for its partnerships with primary care practices within leading health systems in the US. They distinguish themselves by using dedicated nurses to foster trusted relationships with patients instead of relying on call centers. Signallamp seamlessly integrates with existing EHR workflows, facilitating efficient collaboration with care teams. Nurse practitioners, physician assistants, certified nurse midwives, and clinical nurse specialists all play key roles in delivering CCM services and developing care plans.
Additionally, Signallamp’s focus on patient satisfaction and retention contributes to long-term scalability and profitability for healthcare providers.
Timedoc Health
Timedoc Health is a reliable partner for healthcare organizations seeking scalable care management programs. By adhering to best practices and leveraging proven technology, they provide top-tier solutions for integrated virtual care. Developed by physicians, TimeDoc’s care management solutions and services seamlessly integrate into an organization’s EHR system and workflow. The solution supports chronic disease management, care quality, and improved clinical outcomes for healthcare practices.
ChronicCareIQ
ChronicCareIQ is dedicated to enhancing the lives of chronically ill patients through improved communication with their healthcare providers. Their enterprise-ready technology provides a comprehensive software solution for establishing efficient care management programs, reducing reliance on costly third parties. With a transparent pricing model, ChronicCareIQ ensures affordability for medical practices, streamlining patient care efforts and improving health outcomes. The platform also enhances patient education, tracks patient health goals, and improves patient health outcomes.
Choosing the Right Solution
When choosing chronic care management software, healthcare organizations should carefully evaluate the features, benefits, and limitations of different solutions based on their specific needs and priorities. The rise of CCM software underscores a shift towards patient-focused comprehensive care, especially in an era marked by the increasing prevalence of chronic conditions. It is important to support patient enrollment, care plan development, and assisting patients in achieving better clinical outcomes.
Looking ahead, Innovaccer emerges as a leading choice for numerous healthcare organizations. For its advanced data analytics capabilities, comprehensive product suite, and proven track record of success, Innovaccer is committed to continuous innovation. By partnering with Innovaccer, providers can empower themselves to enhance patient outcomes, streamline practice efficiency, and ultimately drive superior healthcare delivery.


.png)



.png)



.avif)









.svg)
.svg)

.svg)

